Doses of Hope

COVID-19 vaccines are all but here. November has renewed our optimism even as new waves of the pandemic continue to ravage many parts of the world. There is now a real chance of a path to recovery in 2021 and 2022.
Three vaccine candidates show promising interim results from their Phase 3 clinical trials. The announcements have come in quick succession.
Pfizer-BioNTech declared 90 per cent vaccine efficacy on November 9th; Moderna followed suit in a week with an efficacy of 94.5 per cent; and Oxford-AstraZeneca came out a week later with results showing at least 70 per cent efficacy, and possibly going up to 90 per cent with the right dosage. While these are early estimates and are subject to revision over time, they are wildly higher than expected. The US Food and Drug Administration (FDA), for example, had only set a 50 per cent efficacy bar before trials began.
Competitive pressure from markets and from governments is immense and not always healthy, and other vaccine developers are racing to announce results and then get regulatory approvals. Vaccine nationalism is also real, with Russia, China and in some ways even India, vying to have homegrown vaccines out. Eight more vaccine candidates are already in Phase 3 trials and the Gamaleya Centre in Russia has issued press releases about the success of their Sputnik V vaccine, but based on smaller and less reliable data. Competition is no reason to cut corners, and vaccine developers, to employ a cliché, need to make haste slowly on vaccines. By and large, the leaders in vaccine development have held themselves to high standards so far.
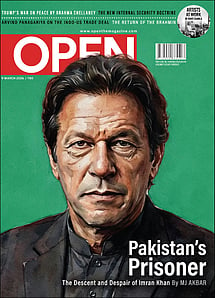
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
It is a remarkable feat that within 10 months of the identification and genome sequencing of the SARS-CoV-2 virus, we have tangible evidence of effective vaccines against it. It is a testament to ongoing scientific efforts across the world that transcend national borders and corporate interests that we have made it this far. The World Health Organization (WHO) lists over 1.25 lakh publications in its Covid-19 database as of November 24th, and the research spans public health, clinical research, basic science and more. A significant number of them have shaped public policy, public health initiatives, the clinical management of Covid-19, as well as vaccine and drug development.
The Mumps vaccine was developed in a record time of four years in 1967, but it had remained an outlier since. The preliminary success of not one but three vaccine candidates in 10 months for Covid-19 would not have been possible if not for the dramatic scientific progress made in the biomedical sciences over the last several decades. This progress comes second only to global advancements in computing and information sciences. An array of reliable, inexpensive and widely available biomedical techniques has been crucial in getting us here.
Before 2020, it would not have been possible to isolate and sequence a virus within weeks of discovering the first infection. It would not have been possible to track how the virus is mutating live during the course of an epidemic and take steps to address it. It is astounding that, as of November 24th, there are close to 2.2 lakh SARS-CoV-2 genome sequences submitted to an open database from around the world. It would not have been possible to quickly characterise the structure, function and dynamics of all parts of the novel coronavirus—from its distinctive spike protein that helps the virus infiltrate human cells, to its nucleocapsid protein that protects the viral RNA from destruction within the human body. It would have been unthinkable to develop and deploy the novel types of vaccines—based on mRNA technology, protein units, viral vectors and more. Many of these technologies seemed like moon shots even six months ago. Just as multiple nations have made it to the moon so far, multiple efforts are becoming tangible vaccines today.
The progress made on vaccines in 10 months can seem like a sprint, a mad dash for protection against this deadly, unpredictable virus. However, the development of vaccines remains a marathon. Being first is not as important as being effective, safe and inexpensive. It is also not a winner-takes-all market, where one vaccine alone can triumph over the rest. A vaccine that may be developed six months to even a year from now could end up having the most impact.
Ironically, it is the continuing spread of the pandemic which has become a perverse boon for how quickly we are getting the results of vaccine trials. Pfizer's story illustrates this well. After promising data on the early safety, ideal dose and immune responses from Phases 1 and 2 clinical trials, they completed enrolling 30,000 people into their Phase 3 clinical trial in September before expanding the trial to 44,000 people.
A vaccine efficacy trial is distinct in many ways from a drug trial, and usually takes much longer. A drug efficacy trial needs to recruit people suffering from an infection or an ailment to test if the drug works. A vaccine trial needs to recruit large numbers of healthy people. Then they need to administer the vaccine candidate to say half or two-thirds of them, and a placebo to the rest. Well-designed trials do this in a double-blind manner where the patient, the doctors and healthcare professionals, and the pharma company do not know more than they need to about who got the vaccine and who did not. Then comes the waiting. Trial participants resume normal lives along with regular checkups, and researchers observe as they catch and report infections.
Typically, only a certain number of people in the study will end up catching the infection in a few months. A vaccine candidate can be declared effective if you find that a lot more people from the placebo group got Covid-19 compared to those who received the treatment. To ensure that the vaccine owner and sponsor do not bias the results, a good trial design lays down in advance how many participants might get infected during the trial period. It is only when the total cases among participants hits that number can the researchers open up and 'unblind' the data and compare who among the infected received treatment and who got a placebo saline injection.
Pfizer's trial design estimated that about 164—roughly 0.5 per cent of participants—might get infected by Covid-19 during the trial period. This becomes a primary 'end point' of the study in declaring the overall efficacy of the vaccine. Moderna had a similar design.
With new Covid-19 cases emerging in the US at faster rates—from 50,000-80,000 infections per day in October to over 150,000 a day in November—Pfizer and Moderna started seeing these numbers being met rapidly. Pfizer and the regulator, the FDA, had planned to open up the data from the interim results when they reached 62 Covid-19+ cases. That threshold was crossed early in November—and by the time they could analyse and present the interim results by November 9th, Pfizer saw a whopping 94 positive cases in its trial. Within the next nine days, this number crossed the 164 target to touch 170. This led to Pfizer announcing the headline results on November 18th, where they could confirm a 95 per cent efficacy, with only eight of the 170 Covid-19 infections occurring among the vaccinated group. Ten of the 170 Covid-19 cases were severe, and only one among them was from the vaccinated group. If the US were more successful in reining in the pandemic, we may have only seen these results by December or January.
The vaccine results are fantastic, but these are also just a beginning. Phase 3 trials have other objectives beyond the primary, such as looking at the vaccine candidate's ability to completely prevent infections, to reduce mortality, to reduce the severity, to examine effectiveness among comorbid and older patients, and more. The vaccine also needs to be safe, and that is why good trials can last as long as two-three years, incorporating data from tracking all vaccinated individuals over the period. While the Covid-19 vaccines will start getting approvals and be used in public vaccination programmes, all approvals remain conditional to no new data coming out about potential harm and dire side-effects that cannot be ignored.
The approved vaccines may still react differently in other countries and other populations. Countries often need to run smaller but important trials among their own populations before deployment. This is already happening in India, with Phase 2/3 trials having commenced for the Oxford-AstraZeneca vaccine adapted by the Serum Institute of India as COVISHIELD.
Dr Reddy's has started Indian trials of the Russian Gamaleya Centre's Sputnik V. These trials are essential, whether they happen before vaccines are rolled out, or parallel to rollout.
THE NOVEMBER vaccine developments also showcase the correct standards for scientific disclosure and openness. The trials of all three successful vaccine candidates so far have been excellent in this regard. While detailed reports and disclosures to national regulators are important, it is also essential to release papers for open, global peer reviews by researchers and free critique of the studies and their limitations. Moderna, for example, has prioritised publishing the studies from their earlier clinical trials in the New England Journal of Medicine. They also released their detailed trial protocol ahead of the trial rollout. This helps avoid cherry-picking the trial results and dilutions in the target objectives. They also enable independent scholars to point out flaws in study design.
The bar set by them has been high, and other vaccine developers need to match them. Many have not done so till date. Russia's Gamaleya Institute has only put out press releases and not shared any reports from their clinical trials with the public so far. In India, Bharat Biotech's COVAXIN has entered Phase 3 trials, but the only research publicly available is on their pre-clinical vaccine studies in animals like mice and monkeys.
The combined successes so far have also underlined another important conclusion: that more vaccines are possible. All the three vaccine candidates focus on the novel coronavirus' most striking physical feature: the spike protein. The spike proteins give the coronavirus their distinctive coronas and are critical in helping the virus enter human cells. The proteins are also attractive targets for sparking our immune systems into action.
As of a November 12th report by the WHO, there are 48 vaccine candidates at various stages of clinical trials around the world, and another 164 efforts in pre-clinical stages. Many of these could be less expensive than Moderna or Pfizer's mRNA vaccines, and may also be easier to deploy in Indian conditions.
All the vaccine news might be great, but can they confer long-term immunity? The trial results could be seen as the vaccines working well weeks after taking them, but six months from now, the data could look worse. Thankfully, we have better answers today about human immunity and Covid-19 than we did a few months ago.
One pressing concern was whether the human body could ever mount a robust immune response to a SARS-CoV-2 infection. Many betacoronaviruses are responsible for the common cold in humans and immunity against them does not last long. Several cases of re-infection by SARS-CoV-2 have also been confirmed now as well. While re-infections remain rare, their likelihood and risk factors all remain unknown and are currently being investigated around the world.
On November 16th, researchers from the University of San Diego published a preprint of an important study on the long-term immunity against Covid-19. They found that overall, many people have a robust immune response up to six months after an infection, even though there is a wide variation in the response. Six months may not seem long, but this is great news given that the virus has only been infecting humans for less than a year. It is certainly possible that elements of this immunity can last well beyond the six months and continue for years.
So how may we gain immunity against this traumatic virus? The adaptive immune system of the human body is formed by both antibodies and by white blood cells like T cells and B cells.
Together, they become our defence mechanism, they remember the first infection or the vaccine shots, and are ready to act rapidly if they encounter the virus in future.
In the best-case scenario, there are high levels of neutralising antibodies that continue to circulate in the blood months or years after the vaccine or the first infection. These antibodies can completely cover any incoming viruses and remove them from the body immediately. They perform a sterilising role—where the virus cannot even cause an asymptomatic infection. But complete sterilising immunity is not the norm, it is simply the immune response vaccine developers strive to achieve.
In the University of San Diego study, researchers found that antibody levels did drop steadily over the course of months and may not be high enough to completely prevent re-infection. The antibody levels arising from vaccines and their long-term levels are being actively studied in many of the ongoing Phase 3 clinical trials, and we will learn more in 2021.
Antibodies are one side of the story. Importantly, the study found that even after antibody levels drop, helper T cells, killer T cells and memory B cells stayed active and circulating in our blood for longer. Killer T cells are capable of immediately killing any human cells that have been infected by the virus, therefore stopping the virus from using our cells to proliferate and attack more cells. Helper T cells can detect low level infections and recruit other parts of the immune system to stop the infection quickly. Memory B cells can start producing the necessary antibodies again after they detect a new infection. So even if antibodies are not there in large numbers the moment the coronavirus infects us, they will be ready in a few days, hopefully in time to halt the progression of the infection to severe disease—which could be a week to 10 days after the initial incubation time of four to seven days, by when the symptoms usually begin to manifest.
Together, this is great news. It means that a future exposure to the virus may result in an infection, but the body will be ready, and can beat it off with mild or even no systems. With good vaccines, Covid-19 may become yet another throat infection. This may not hold true for everyone, but if it holds true for large numbers of people, then widespread vaccination can effectively rule out further epidemic-scale waves.