Left Alone
The psychological toll of recovering in isolation
 Nikita Doval
Nikita Doval
 Nikita Doval
Nikita Doval
 |
07 Aug, 2020
|
07 Aug, 2020
/wp-content/uploads/2020/08/Lefalone1.jpg)
(Illustration: Saurabh Singh)
On his first evening in the ICU, Ismail Dean, 22, thought his cousin was lying beside him. Only it wasn’t the living breathing brother he had grown up with, but the way Dean saw him last: a lifeless body in a cloth bag. “I started panicking and I looked up and everywhere around me were only bodies of Covid patients. It was a pile and I was stuck in it.” What Dean experienced that night was a bout of hospital delirium, common among older patients, particularly those in the ICU. But now, it is increasingly being seen in Covid-19 patients such as Dean. Extreme anxiety and isolation from any human interaction—the medical staff attending to you in PPEs only reinforces that isolation—are some reasons why patients are experiencing these hallucinations, leaving them scared, even after they have tested negative.
Dean’s stint in the ICU at Nichani hospital in Chennai lasted only three days. Now, the business executive is back at his home in the city. His last Covid-19 test came back negative and he’s looking to resuming his life again as his home isolation has ended, but fear persists. “I spent so much time worrying about who all I would have infected as I was absolutely asymptomatic till my test came back positive in the first week of June.” He had been making errand runs, albeit with gloves and masks, and fretted over everyone he might have come in contact with. He wanted his sister to retrace his steps, from petrol pumps to grocery stores, to warn everyone. “What if I killed someone? Added to this was the guilt of bringing the virus home—my father had also tested positive. My partner became very evasive when I broke the news, was reluctant to talk. My friends dismissed my diagnosis as a joke and then when they realised I was serious, they stopped taking my calls. It was almost as if they feared catching the infection.” Dean is in fact convinced that it was emotional turmoil that worsened his condition leading to his stint in the hospital. His breathlessness started a day after his partner and friends avoided his calls. “I feel that if I had got the required emotional support, then I would have never had to go to the hospital. My father remained asymptomatic throughout. For me, the emotional cost of the infection was more intense than the physical one.”
Dean is not the only such Covid-19 patient. Increasingly, the biggest challenge for those who are diagnosed positive but are only mildly symptomatic is the psychological fallout. From isolation in windowless rooms on empty floors almost menacing in their eeriness to feeling completely friendless and alone in an alien city to crushing anxiety even when locked in your own home with your family just a few feet away, men and women across the country are finding that it is their emotions they have to be the most careful of.
“For me, it was not a matter of if but when I will catch the infection,” shares Dr Syed Faizan Ahmad, 25, a general surgeon at Silchar Medical College in Assam. Ahmad has only recently moved to Silchar and by his own admission had not settled in enough to make friends when he was put in isolation for 14 days. “I took the news of my diagnosis very well, in fact I actually thought I could work in the isolation ward.” But the reality was quite different. Ahmad’s situation remained stable throughout, but anxiety was his companion from the minute he walked into his room in the isolation ward. “You would think that things that you enjoy—social media, movies—will keep you busy, but no. Your room is a prison cell and you endlessly pace up and down. You crave human contact.” Ahmad chose to not tell his family in Etawah, Uttar Pradesh until the fifth day of his diagnosis when he was sure that his condition wasn’t going to worsen. His first phone call to them was like water to a parched man.
Extreme anxiety and isolation—the medical staff attending in PPEs only reinforces that isolation—lead to patients hallucinating and scared even after they have tested negative
It has been over four months since Covid-19 was declared a pandemic, but our knowledge of the disease, its expressions and even how the infection travels is still changing almost every day. Pandemics are as old as time and yet this is an unprecedented situation for almost everyone alive today, historical pieces about the Spanish influenza notwithstanding. “There is a generalised sense of vulnerability and worry. There is significant uncertainty. So even before people are affected by the virus they are affected by the Covid narrative of isolation and helplessness,” says Dr Achal Bhagat, psychiatrist, Indraprastha Apollo Hospital, Delhi. The extreme narrative built around controlling the disease, from lockdowns to sealing apartments and colonies puts people further at edge. “The emotional impact of all this starts becoming evident in the form of loneliness, fear, anger and self-blame,” says Dr Bhagat. At its worst, this can manifest itself in suicides, as are being reported from across the country. More and more hospitals across the country are now introducing counselling for Covid-19 patients.
Medical science has time and again proven how important social interaction is for not just our mental but also physical health. “Human empathy and contact are very important during the time of a health crisis. The immune system responds faster if loved ones are around. Even in the most critical of diseases, a patient is never alone unless it is required medically. But that is not the case with Covid,” says Dr Nikhil Modi, a pulmonologist with Apollo Hospital. For instance, Dr Ahmad realised this the first time someone walked into his isolation room. “I had been wearing a PPE kit on my rounds and I never gave a thought to what it might be doing to patients until I was on the other side.” As a doctor, he says, patients will pick cues from your expressions when you talk to them. They feel reassured by your tone, eye-contact. There is a greater give-and-take. A PPE kit renders a medical staffer completely unapproachable. “Till the person would speak I would not even know what their gender was.” He is scheduled to start his rounds this week and has promised himself that when he talks to Covid-19 patients this time, he will make more of an effort.
That is certainly reassuring for Rohit Sachdeva, a radio show host with a Delhi-based channel. Known to his audience as Yuvi, Sachdeva was admitted into a hospital when he suspected he was Covid-19-positive. Quarantined for two weeks in the Philadelphia Hospital in Ambala, Punjab, where his family is, he isn’t even sure if there was anyone else on the floor. “The room was windowless. Every day I would walk 60-70 steps to pick up my food which would be left at the end of the corridor and the only person I saw was the doctor. But if you asked me to identify them, I wouldn’t be able to, because I never saw their face.” Sachdeva’s major symptom was a persistent stomach ache and while he knew there wasn’t anything to worry about, the isolation made him think otherwise.
Distress during an illness often leads to psychosomatic symptoms. A development professional who did not wish to be identified spoke about how his resting heart rate was higher by almost 20 counts every time he checked but the doctors told him that it was probably his body’s heightened reaction to his anxiety. “Till date I don’t know if it was an actual symptom.” He finally tested negative after three weeks of home isolation in the first week of July but says that even on the road to recovery, every small thing would make him worry. “For instance, I would wake up parched in the middle of the night. It’s such a small thing that you wouldn’t even think about in ordinary times. But for me it could well have been another symptom,” he says.
While the world has been alert about the dangers of Covid-19, its impact on mental health remains underemphasized despite warning from experts. In fact, within a week of the lockdown in March, the Indian Psychiatry Society had released a survey stating that the number of reported cases of mental illness in India had risen by 20 per cent. Economic distress and uncertainty about the future compound the problem.
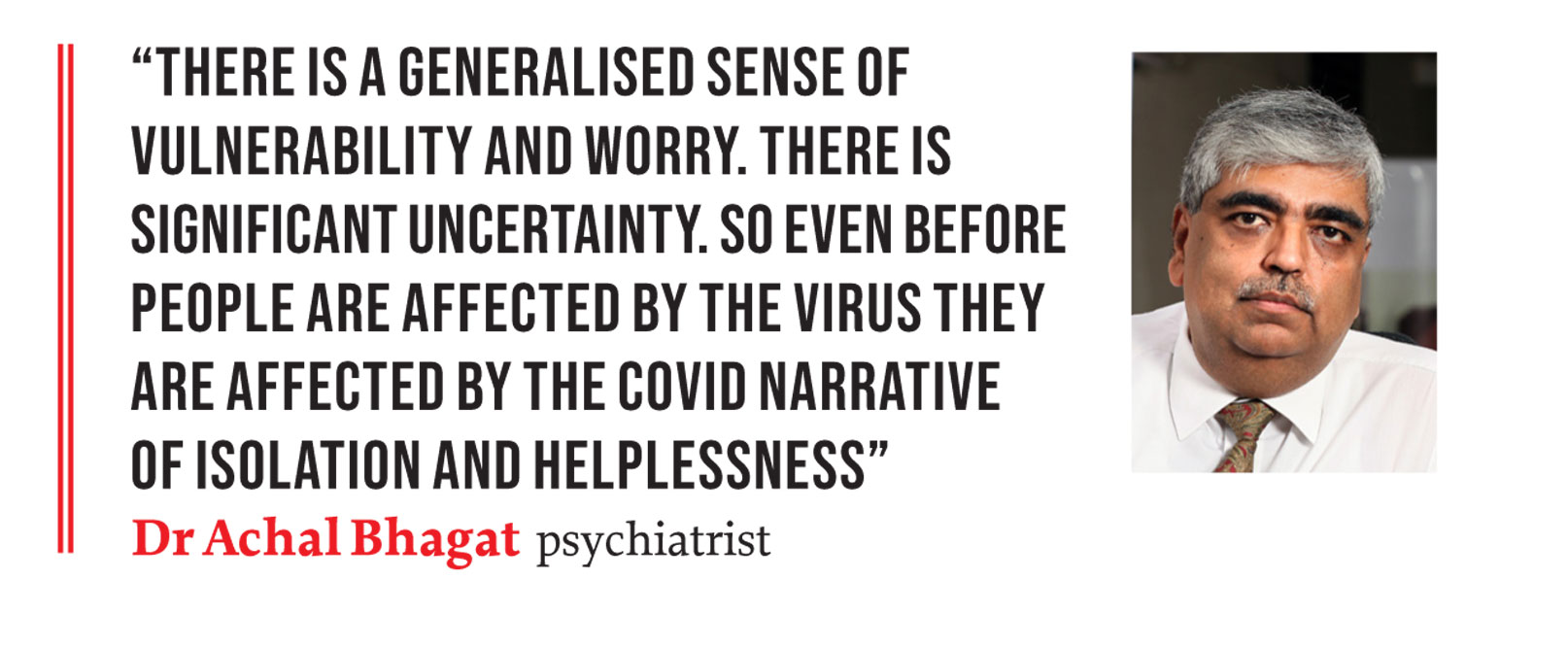
The narrative around the Covid-19 remains centred on those who succumbed to it, including healthcare professionals who died in the course of attending to patients. Milder cases, while a well-documented fact, don’t occupy the same mindspace in the public discourse. “People who survive without an event do not have reason to spend time countering the narrative. Many who do speak of recovery sometimes broadbrush the nuances of the experiences and describing these could be retraumatising,” says Dr Bhagat. In an ideal world, there would be a non-judgemental caring health system, but right now it is “inflexible, distant and bureaucratic”, he says. Patients are aware that their families cannot be with them, but the absence still rankles. Dean says he was upset with his mother for not coming to see him even though he knew she had to be with his father (who was home-quarantined) and the lockdown would have made it impossible for her to come. “The practical side of me knew what the problems were, but I still felt abandoned.” Usually, in hospital wards patients end up forming bonds with each other, exchanging notes on health and life, but that is not the case in a Covid-19-struck world. “Such is the fear that Covid patients feel if we interact with each other, would we end up jeopardising our recovery? Maybe my strain is weaker and the other person’s is not? All of this makes the experience very difficult,” says Dr Ahmad.
Quite a few of the patients Open reached out to spoke about how consumption of news and social media made the experience tougher for them. Both Dean and Sachdeva were in isolation when the actor Sushant Singh Rajput killed himself. Both mentioned how it shook them up completely, adding to their sense of despair. “Frequent checking of symptoms, the narrow focus on [those] who did not make it, all these contribute to a potent cocktail. It is best to keep your phone aside when not talking to people. In fact I would go a step further and recommend that this is all you use it for, talking to people,” says Sachdeva.
Nearly everyone Open spoke to has recovered, with a few being in the last days of their quarantine. The reaction of people around them has been an eye-opener though, because most do sense hesitancy in friends and family in coming in contact with them. Dean reveals how an uncle refused to let his wife’s body come home. Sachdeva’s home quarantine ended on July 10th. He now wants to make a video detailing his experiences for social media to address the fear, uncertainty and, yes, the stigma around the disease. “If more and more former patients speak up, it will help destigmatise this as well as offer moral support to those who are currently positive.” The Telangana government is in fact considering asking former Covid patients to step up as volunteers for counselling, while in Chennai, a support group has sprung up of such patients to provide counselling.
At the time of going to press, India had 19 lakh cases of Covid-19. A serological survey conducted in Delhi has found that one in every five individuals has antibodies, indicating the presence of a large number of asymptomatic patients. The fatality rate however continues to be low. It has been argued that the country could have a milder strain of the virus though there is no evidence to back this. What could have played a role is that the bulk of India’s population is considerably younger. While most people who have been infected mildly and have recovered will also go on to leave the trauma of their one month or few weeks of isolation behind, the larger looming problem of mental health cannot be ignored. “Diverse groups of people are likely to have mental health needs related to Covid-19. From those who have suffered but recovered, to those who may have unfortunately lost someone to children growing up in these times, everyone may need access to mental health skills to cope. And for that we need to move away from the stigma of seeking help for mental health. It does not have a vaccine,” says Dr Bhagat.

/wp-content/uploads/2025/07/Cover-Shubman-Gill-1.jpg)












More Columns
‘Fuel to Air India plane was cut off before crash’ Open
Shubhanshu Shukla Return Date Set For July 14 Open
Rhythm Streets Aditya Mani Jha