Not Quite Polio-free Enough
Why India’s strategy to combat polio is mistaken
 Kalpish Ratna
Kalpish Ratna
 Kalpish Ratna
|
01 Aug, 2013
Kalpish Ratna
|
01 Aug, 2013
/wp-content/uploads/2015/11/polio2.jpg)
Why India’s strategy to combat polio is mistaken
Two days ago, when I picked up the newspaper, I found myself in a time warp.
It was still Sunday, still 8 am, but dark as midnight outside. It had rained nonstop for twenty-four hours. The lights had failed. I was in a room lit tipsily by a powerful torch held up by a well-intentioned but very drunk ward boy. He was trying hard to focus the beam, but his hands shook—perhaps not from the alcohol, but from fear.
I was terrified too.
Stretched flaccid and helpless between us was a two-year-old girl who had stopped breathing minutes ago.
My job was to do a tracheostomy on her, make a small slit in her windpipe and hook her to a ventilator.
That was soon done, her tiny chest was set moving again, but the worst was yet to come.
As I straightened up, the child’s unseeing eyes held mine with the question: Why did this happen to me?
This was bulbar polio—poliomyelitis affecting the brainstem.
The little girl’s brain was targeted by a virus that, more usually, attacks the spinal cord.
Her bewildered parents protested, “But we did give her the vaccine! How can this be polio?”
I had no answer then.
The year was 1983.
This is 2013, and I am reading of a child who asks the same question—a child who is deeply unconscious and paralysed. Her parents have the same question.
Do we have an answer now?
Yes, we do.
But it cannot be said out aloud.
The parents are likely to hear this instead: “It is very rare for a vaccinated child to suffer paralysis. Only one in 1.4 million vaccinations!”
How does that matter to these parents? To them, their child is the rarest of the rare, she is unique, she is their own. She is the only child on the planet who matters to them. At this moment they don’t give a damn that the other 13,99999 vaccinated children are fine. Their child is paralysed, their child may die.
When you are faced with one paralysed child, that child and that child alone becomes the face of the disease. She represents all of poliomyelitis, the sum total of research, discovery, invention and prediction about this disease. She becomes the template that must dictate all our strategy.
Here she is: a two-year old girl on a ventilator, paralysed in all four limbs, because she is infected with a Vaccine Derived Poliovirus.
Here she is, and, what are we going to do about it?
Poliomyelitis is caused by an enterovirus. It is a single strand of RNA in an icosahedral (20-sided) shell of protein. Infection occurs when the virus is swallowed with food or water. It resists stomach acid, latches onto the lining of the intestine, and replicates. From the intestine into the blood stream is a quick transit, and very soon the virus circulates through the body’s muscles. From the nerve-muscle junction, the virus travels along nerves into the spinal cord, and sometimes into the brainstem. Weakness in the limbs, leading to paralysis, is the result.
Poliomyelitis, literally, is ‘inflammation of the grey nervous tissue’, a label the disease acquired in 1874, when the site of affliction in the spinal cord was first discovered.
Throughout the course of the disease, and for weeks afterwards, the patient sheds poliovirus in the stool. It spreads from person to person through faecal-oral transmission—when you swallow food or water contaminated by infected faeces. Very common, almost unavoidable, in a country where less than 50 per cent of the population has sanitation.
Poliomyelitis is a disease caused by an enterovirus, but it is equally a disease caused by the virus of apathy, fatal in a country as poor as ours.
Polio does not make a dramatic entry in most cases. Often, the first sign in a child is paralysis. The euphemism AFP, heard more often than the dread word ‘polio,’ paradoxically tells the worst story. Acute Flaccid Paralysis translates as ‘sudden paralysis’ that leaves the limb (or limbs) floppy and useless.
While every case of AFP may not be due to poliovirus, most are. So why not call it the polio it is?
Shhhhhh! Polio is supposed to have been eradicated.
Most viral diseases have no cure. All medical science can do is address the symptoms and consequences of infection. No matter how we dress that up, it only means that we can do very little. Our strategy against poliomyelitis must therefore concentrate on defence. How can we prevent polio?
In 1983, when I confronted my first case of bulbar polio, it was nearly 30 years into immunisation. There was still a lot of polio around then. One of the greatest joys in paediatrics has been to witness the wane of poliomyelitis. Going, going, we told ourselves year after year, and yet it isn’t quite gone. And to the doctor who sees even one case, the disease seems unchanged.
But it has changed, and especially, in that one rare case.
If we are to eradicate polio, it is that change we must confront.
To understand that change, we need to find out more about the poliovirus.
Unlike many other viruses, it affects only primates, and there is no known natural reservoir. This means the poliovirus is not napping in some other species, waiting to make the leap to Homo sapiens.
Three forms of poliovirus are known—types 1, 2 and 3. All three are ‘wild,’ or exist in nature. Countries where polio is constantly present in the population are termed ‘endemic.’ Till recently, India was among them.
In endemic areas today, Types 1 and 3 are the infecting strains of poliovirus. Type 2 is believed to have been eradicated; it was last isolated from a case in Uttar Pradesh in 1999. Both Type 1 and 3 can cause paralysis.
Any vaccine that prevents poliomyelitis must be effective against all three strains in order to prevent paralysis.
The first vaccine to be introduced was the Inactivated Poliovirus Vaccine, also called the Salk Vaccine, after its originator. Since its introduction in 1954, IPV has been implemented in Europe. That continent is now polio free.
IPV is an injectable vaccine, and was thought difficult and unfeasible for use in the immunisation of the masses in developing countries. In the next two decades, it was also thought (wrongly), that IPV was poor protection in endemic areas.
In 1978, when the caseload of polio in India was around 500 cases per day, India chose the Oral Polio Vaccine, administered as oral drops, for mass immunisation. Three doses of the vaccine were then recommended. OPV, developed in 1961 by Albert Sabin, contains attenuated (weakened) live poliovirus of all three wild strains. The body responds by developing antibodies against all three strains to protect against infection.
OPV has one (questionable) advantage over IPV: it induces ‘mucosal immunity’ in the intestine. It prevents wild strains from replicating in the intestine. This means, hopefully, that a child immunised with OPV will not spread wild poliovirus by shedding large amounts of it in the stool.
But, after immunisation, the child will shed a lot of ‘vaccine poliovirus’ in the stool.
It was hoped by a lazy government that India’s lack of sanitation might actually prove useful in conferring ‘herd immunity’ as the ‘vaccine poliovirus’ would spread through faecal-oral contamination.
Lazy? That’s too mild a word. Culpable is more apt.
Three doses of OPV should confer lifelong immunity against all three strains of poliovirus, and the statistics say this happens in 95 per cent of cases.
That is just statistics.
In truth, for the first ten years after OPV introduction, there was no great improvement. At best, the efficacy was 70 per cent. It was assumed that to step up efficacy, at least six to 10 doses of OPV were necessary. The ‘herd immunity’ OPV was fondly hoped to provide, through lack of public sanitation, also did not materialise.
The WHO’s Global Polio Eradication Initiative (GPEI) was launched in 1988. Its goal was eradication by the year 2000, and certification (the absence of wild-type virus for at least three years) by the year 2005.
In 1995-96, India joined this global effort, and the Pulse Polio Programme was pushed. By 2000, when we should have been polio-free, the goal was nowhere in sight.
In 2004, health professionals presented a memorandum to the WHO, The Global Polio Eradication Initiative and the Government of India pointing out that the present strategy was not working. There were still wild poliovirus infections resulting in paralysis—and many of these in children who had been immunised. More disturbingly, it also underlined the occurrence of Vaccine Associated Paralytic Poliomyelitis in the decade since the GPEI.
This was, perhaps, the first time it had been publicly stated that Vaccine Associated Paralytic Poliomyelitis (VAPP) is commoner than expected.
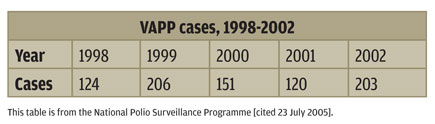
As far back as 1999, India had 181 cases of VAPP.
How does VAPP occur?
You might want to look at it thus: how can VAPP not occur? OPV is a live vaccine—attenuated, yes, but live. Its very attenuation is an evolutionary prompt for it to mutate. Given the nature of the beast, its fight for survival in the host would make it mutate into a more virulent form. A Vaccine Derived Poliovirus is as if not more likely to cause paralysis as a wild strain.
In 2006, around 1,600 cases of VAPP were reported while the mass immunisation programme was at its pitch; how could they possibly be overlooked?
They were not. Paediatricians and epidemiologists have repeatedly raised angry voices against a strategy that depends entirely on OPV. Their recommendation, right from the mid-1990s, has been to include the Inactive Poliovirus Vaccine, the injectable IPV, in the National Immunisation Schedule.
IPV cannot cause paralysis as the virus is inactive and so it cannot mutate. Its only drawback is that it does not cause ‘mucosal immunity’ in the intestine. This means that ‘herd immunity’ in areas with poor sanitation is not possible through IPV. Translated, this means that children immunised with IPV will not ‘shed’ weakened vaccine virus in their stool, and so will not transmit immunity by contaminating food and water with their faeces.
Think of it; it is a horrendous thought. It also feeds into the old chestnut that poliomyelitis once was a ‘White Man’s disease’ and we smart Indians escaped it by defecating along the roadside.
Sorry, but that is wrong: India had endemic polio in towns and villages without indoor plumbing.
That argument against IPV does not hold water. The only other argument against using IPV is the cost and that it is not manufactured in India. Why not?
If the Indian Government is still buying into the WHO idea that OPV is the best choice for mass immunisation, how will we argue away VAPP?
Let’s look at what we have to argue away: a nine-month-old boy from Thane, a ten-month-old boy from Beed, both in Maharashtra; an eight-month-old boy in Kalahandi, Odisha, a five-month-old girl in Jehanabad, Bihar—all of them have suffered VAPP this year. They hardly count as statistics—unknown, unnamed as they are—but what if it were your child?
That is not a question Indian policymakers consider.
Right now, they are in the race for certification as a polio-free nation. Right now, India is looking good on paper. The National Polio Surveillance website has an anodyne explanation for VAPPs. It just fails to mention that we are ignoring the near-universal strategy of including IPV in our Immunisation Schedule.
It also fails to mention that the people who actually deal with polio—paediatricians—are shouting themselves hoarse that we are not free of polio. True, the pockets of wild poliovirus infection predominate in areas where mass immunisation has failed. Isn’t that because these areas have polio despite OPV?
Isn’t that also because our perceptions are coloured by injustice? Aren’t these also areas that governments have targeted with draconian force and pogroms?
How can mass immunisation be perceived but as a method of coercion and control?
The events of Abbottabad are now fodder for Hollywood and Osama bin Laden rightly resides in the dungheap of history. By now everybody knows the story of Pakistani doctor Shakeel Afridi who was used by the CIA to pose as a vaccinator and collect Bin Laden’s DNA. As a result, all immunisation is suspect in the Af-Pak corridor and children are once again victims of polio.
Every time science is deployed as a political weapon, the distrust it engenders is violent and absolute. It subverts and criminalises the ethic of medicine. We might escape its consequences, but our children will not.
Surgeons Ishrat Syed and Kalpana Swaminathan write together as Kalpish Ratna. Their most recent book Once Upon A Hill is about the lost hills of Bombay

/wp-content/uploads/2025/07/Cover_Dalai-Lama.jpg)









More Columns
Gukesh’s Win Over Carlsen Has the Fandom Spinning V Shoba
Mothers and Monsters Kaveree Bamzai
Nimrat Returns to Spyland Kaveree Bamzai