A Shot of Hope

It is hard to quantify hope, but on the morning of January 12th, it had a shape—a glass vial of just 5 ml capacity filled with a transparent liquid: the Covishield vaccine. It was being carried in three pharma trucks that rolled out of the Manjri premises of the Serum Institute of India (SII). By 7:23AM, Pune airport's Twitter handle had posted a video of the boxes being placed on a conveyor belt, with the message 'Stand by India!' Each box had 'Rush Vaccine' stamped on its side apart from the legend 'May all be free from disease' in English and Sanskrit. By 4PM, more than 54 lakh doses of Covishield had travelled across the country according to the Union health ministry.
The country's capital was one of the first cities to receive its instalment, more than two lakh doses, by 10AM that day. But even before the SpiceJet flight that was carrying the vaccine took off from Pune, anticipation hummed through the corridors of the Rajiv Gandhi super specialty hospital in East Delhi. "If vaccine is gold then we are RBI," laughed Dr Chhavi Gupta, media spokesperson of the hospital. In late November itself, the Delhi government-run hospital was identified as a vaccine storage facility and since then work has been on here in full swing. A three-storied utility building in a secluded corner of the hospital campus was identified, a few metres away from a gate so that entry and exit of refrigerated trucks and vans could be facilitated. The building has been taken over by the state government's health department. On the day Open visited the site (before the arrival of the vaccines), security guards questioned those who were within walking distance of the building even as life-size Godrej crates were being placed side by side. "There is a CCTV room and the storage facility will be manned 24 hours, to maintain inventory and security," says Gupta. The hospital will play no role in the handling of the vaccine.
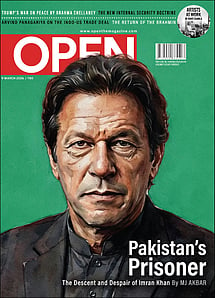
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
Sushila, a healthcare worker at the Gayatri Hospital in Uttar Pradesh's Ghaziabad district, usually reaches her workplace by 9AM. But on January 16th, she will be there at least an hour earlier. "I am not even sure I will be able to sleep, out of both nervousness and some excitement too," she laughs. It is on this day that one of the world's largest immunisation programmes will roll out as India begins the project of vaccinating its billion-plus population against Covid-19.
A gigantic project involving 19 ministries and all the lessons garnered over three-and-a-half decades of the Universal Immunisation Programme (UIP), this vaccination drive will test just about every system the country has in place, from transportation to last-mile rural health coverage. The first phase will see the vaccination of three priority groups: healthcare workers, frontline workers, who include personnel from state and Central police departments, the armed forces and even municipal workers, and people above 50. Those under 50 but with co-morbidities will also be included in this phase. The Government aims to vaccinate 30 crore people by summer of this year. To put it in perspective, a little over two crore people have been vaccinated worldwide since December when the UK became the first country to start vaccinations. The list of healthcare and frontline workers have already been provided to states and Central ministries from the data sent by health institutions and uploaded on the Co-WIN platform. The aim of vaccinating those on the frontlines is well-thought-out so that services do not falter, according to Srinath Reddy, president of the Public Health Foundation of India.
Of all the vaccines that have been approved for use all over the globe till date, there are three manufacturers whose vaccines have been the most anticipated: Pfizer, Moderna and AstraZeneca. In India, two vaccines have been given emergency approval: Bharat Biotech's Covaxin and Covishield, which is a result of SII's tie-up with AstraZeneca. Obtaining the vaccines may have been the easiest step in the long march that should culminate in the defeat of the pandemic. From cold-chain logistics to trained vaccinators, from the correct messaging to adequate security protocols, the Union and state governments face the unenviable task of pulling off a globally unprecedented exercise. The health ministry itself acknowledges in its operational guidelines that 'the highest level of political and administrative ownership, commitment and support is vital for successful planning and implementation of Covid-19 vaccination.'
Dry runs have been conducted across districts to simulate actual vaccine administration with the election process serving as a blueprint. Each site will administer the vaccine to 100 beneficiaries every session which in turn will be managed by a five-member team. A text message will inform the beneficiary of the time and place when and where they will first encounter Vaccination Officer 1—a police or home guard personnel who will be in charge of pre-checking the registration status of the beneficiary as well as verifying his or her photo ID. "Once inside, the beneficiary's document will be verified in the Covid Vaccine Intelligence Network (Co-WIN). Social distancing norms are to be followed at every step of the way," says Dr Sanjay Agarwal, Additional Chief Medical Officer of Ghaziabad. The actual vaccination will be carried out by a trained vaccinator even as support staff uploads the details on the Co-WIN app. After vaccination, the beneficiary will be taken to a third room for a 30-minute monitoring of any After Effects of Immunisation (AEFI) before he/she leaves the premises. Text details of the second vaccination date will be sent in real time to the beneficiary. All of this, including the monitoring, is standard protocol during vaccinations, says Agarwal.
In the dry run that was conducted on January 11th, Sushila was the vaccinator while her colleague Subhinesh was in charge of uploading the information on the Co-WIN app. "The first couple of shots took over five minutes mostly because of nervousness even though this was a drill and I have been a vaccinator for three years now," says Sushila. But once she found her groove, it was smooth sailing. Subhinesh, too, struggled with the app but it is precisely to identify these issues that the dry runs were conducted. States such as Maharashtra have identified internet connectivity and even inadequate health services in rural areas to deal with possible AEFI-related complications and have recommended that data be uploaded offline as well. Health experts have also raised similar concerns along with the possibility of there not being enough trained vaccinators as the drive expands. As it happens, both Covaxin and Covishield are intramuscular injections.
Co-WIN is an extension of the electronic Vaccine Intelligence Network (eVin) launched in 2015 for the UIP and is meant to facilitate every aspect of vaccine distribution, from maintaining digital records of usage and available vaccine stocks, as well as monitoring temperature. The app, which will be available to the larger public only later, will also allow the monitoring of utilisation and wastage of the vaccine as everything, from the batch number of the vial to doses utilised per vial, will be uploaded on it. The app will come alive at 9AM and shut off at 5PM, keeping a tight control on vaccination schedules.
One of the biggest challenges in this battle is the maintenance of the cold chain. UNICEF defines it as a 'chain of precisely co-ordinated events in temperature-controlled environments to store, manage and transport.' Both Covaxin and Covishield require temperatures between 2 to 8 degrees. One of the main reasons why Pfizer remains a vaccine for rich countries is because its temperature requirement is (-)70 degrees and this needs specialised freezers that can cost anywhere between $10,000 and $15,000. According to figures cited by Union Health Secretary Rajesh Bhushan, in a briefing made on December 15th, 2020, India currently has more than 28,000 cold-chain points apart from 240 walk-in coolers, 70 walk-in freezers, 45,000 ice-lined refrigerators, 41,000 deep freezers and 300 solar refrigerators, which will be used for storage of Covid vaccines. At centres where vaccination is taking place, the vaccine will be kept in cold boxes with the lid closed till the beneficiary enters the premises. At the end of the day, all unopened vaccine vials are to be sent back to the distributing cold-chain point. The ones returned from the previous day have to be marked and stored separately so that they are used first on the following session day. The date and time of opening a vial must be carefully recorded and an open vial will have to be discarded after four hours of having been opened.
SII has said that they already have 500 lakh doses of the vaccine ready although the group also has commitments to other countries. Bharat Biotech has an initial order of more than 50 lakh from the Government and is confident that they can manufacture 7,000 lakh vaccine doses by the end of the year. Whether vaccine shortage will become an issue in the days to come remains to be seen but there is an urgency to ensure that additional medical supplies like syringes and gloves are available in adequate numbers. Covid-19 may have been declared a pandemic only in March last year but Rajiv Nath, managing director at Hindustan Syringes & Medical Devices, the manufacturers of Dispovan syringes, knew in February itself that the company would have to expand its manufacturing capacity. Thanks to India's immunisation programme, there is an adequate supply of 0.5 ml intra-muscular syringes of the auto-disable variety. It is the same syringe that is required for the Covid vaccine. Nath says the Government only woke up to the need for more syringes in September last year, asking syringe-makers to ramp up their manufacturing capacity. "I knew that we would have a vaccine but unless we ramped up production early on, there might be a problem of enough doses being available but not enough syringes to deliver them." With over 30 crore intended beneficiaries in the first phase itself, the requirement goes up to approximately 70 crore syringes. By June 2021, the company is on target to raise its production to 100 crore pieces, but like SII, it too has international commitments. At this stage however, Nath does not foresee a shortage unless the Government clears the private sector for administering the vaccine.
India's UIP is widely considered to be one of the success stories of global immunisation and comparisons between its success and the Covid vaccination drive are inevitable. But Dr Suneela Garg, a public health expert, says that there was a lot of struggle at the beginning of that programme too. "There were myths and misconceptions then as there are now. These need to be countered at every step of the way." The mindset of teeka lagana hai (a vaccination shot) has entered the psyche of at least the mother in the country says Shailaja Chandra, a former secretary with the Union Government. "When UIP was first started, there were naysayers who balked at the thought of setting up cold-chain supplies in states like Bihar, but we have built systems and structures in place. Even as early as March we were spreading the message about Covid through ASHA and Anganwadi workers and that helped create awareness," she says.
From election rolls to Census data to satellite imaging, every resource at the disposal of the Government needs to be called in for this drive and Chandra says it already is. The loss of income brought about by the lockdown instilled a fear of the disease in people's minds. India is increasingly reporting fewer Covid cases on a daily basis despite consistent testing. Yet, this should not make us complacent. "Rich people have the ability to remain secluded, but the ordinary man has no such luxury. He has been hit once and as such there shouldn't be resistance," she says.
The second phase of vaccination will ideally be meant to provide herd immunity but a lot of factors will ride on its success, beginning first and foremost with the stage the pandemic is in. "Will it be raging? Will it be receding on its own? These questions will have to be taken into account when the second phase is being planned. More than a crore of infections have come to our attention but there would have been several lakh silent ones also so that cohort has memory cells. Questions like would only people above the age of 18 be vaccinated will need to be answered. But before we address all of that, we have to ensure the first stage goes off well," says a public health doctor who does not wish to be identified.
January 16th will begin with a prayer on everyone's lips, the answer to which we may not fully receive for months yet because, like intelligence operations, the success of a public health initiative is usually not visible for years. But by the time the first phase draws to a close, India should have some answers as to how the pandemic is likely to fare in the second half of 2021.