Cancer in the Time of Covid-19

The initial reaction of cancer specialists, or oncologists, worldwide to the pandemic as well as the subsequent course corrections, once patient numbers began to fall, have been out of routine. Rather than relying on data based on proper clinical trials and articles that have been peer reviewed, oncologists by and large were ready to base their clinical judgements on experiential data coming out of China and Italy, among other countries affected by the virus. The estimates of cancer patients who had fallen victims to Covid-19 went as high as 30 pert cent with little or no reference to type and stage of cancer, age and health status of the patient, etcetera.
Consequently, cancer hospitals more or less shut down their facilities asking patients to stay at home. Outpatient departments were closed, appointments were cancelled, chemotherapy treatments were delayed, only emergency surgeries were being done while checkups and screening programmes were put on hold along with clinical trials. This excessively cautious reaction was puzzling as oncologists know full well that at any time those they treat are at risk of dying of infections, if not from the side-effects of their toxic treatments. What had changed so drastically?
A doctor in the US, on the frontline of fighting Covid-19, put it well when he said, "We are spooked." Spooked by a virus that has been relentlessly covered by the media as a killer coming to get you. Psychiatrists have already coined a term to describe this state of mind: pre-traumatic stress disorder. While the threat is real, and I fully understand the stress our frontline care providers are facing, I would like to draw attention to the high levels of anxiety being suffered by people with cancer who are being told not to come to hospitals for further treatments as they may contract the virus . Instead, they are being encouraged to use telemedicine to consult with their doctors from a safe distance. Which brings me to the next set of questions.
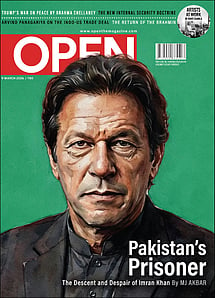
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
Is it not the responsibility of medical establishments to ensure that proper precautions are taken so that their patients are not at risk of contracting the virus when they come in for their treatments? Surely in cancer treating hospitals this should be the norm as their patients are immune compromised anyway? During the SARS outbreak in Toronto, Canada, precautions were taken to triage patients at the door and ensure that anyone who entered did not have fever and had followed proper sanitary guidelines. They were also advised to visit without a companion. And SARS, as we know, was a far deadlier killer than Covid-19.
There is an even bigger question which pertains to the nationwide lockdown. Did anyone think of what this would do to patients with serious illnesses and severe chronic conditions, and this does not include only people with cancer who depend on public transport to ferry them back and forth? Not only can they no longer come in for treatments but they are also being deprived of essential medical supplies. A few examples from media coverage and our own experience at CanSupport (a free palliative care service for cancer patients) should suffice to illustrate how desperate the situation is.
Recently, we heard about the 65-year-old farm labourer, Arivazhagan, from Tamil Nadu, who pedalled 140 kms to bring his wife, Manjula, to the regional cancer centre in Puducherry for her third cycle of chemotherapy. A well-known journalist also highlighted the plight of a poor man with cancer of the upper lip who walked several miles, on foot, to LNJP hospital, to find that it had been turned into a facility for Covid-19 patients only. The patients waiting on the footpath outside our major cancer centres is of course legendary. You may well ask why don't these people go to the nearest government hospital near their homes and why don't they call or use telemedicine to fix an appointment with their doctor as is being recommended?
The trouble is, based on their experience in the past, people like Arivazhagan and Manjula don't trust government hospitals and have never heard of telemedicine. Besides, district-level hospitals, by and large, have neither the expertise, facilities or medicines to treat cancer patients. Chemotherapy treatments given by IV have to be carefully administered and supervised by a trained practitioner. Nurses, too, should know how to prepare and mix these drugs as a slip up can cost a life. Neither do these hospitals have radiotherapy facilities. So, here comes a pandemic that warrants a lockdown and unless you live in a metropolitan centre or a big city, you are left helpless. But all is not lost. Where there is a will, there is a way.
Odisha is an example of a state that has reacted positively to solve the problems being faced by cancer patients, which were brought to its attention by local cancer support groups. Not only did they widely publicise contact numbers of hospitals and doctors but also arranged for chemotherapy to be made available to patients in every district hospital in all 30 districts of Odisha. These hospitals were in turn connected to the Regional Cancer Centre at Cuttack so that oncologists based there could guide the treatments and ensure both efficacy and safety.
Understandably, at present, the anxiety levels of people who anyway are battling diseases and medical conditions with uncertain outcomes is very high. It is not difficult to imagine the plight of someone who has been told in the past that their ability to fight cancer lies in their adherence to regular treatment protocols now being told that their next round of treatment has been postponed indefinitely. Even when there is consultation between patients and their practitioners, often the former come away feeling that they may have made the wrong decision, which only adds to worry.
Not surprisingly, the CanSupport helpline, where people affected by cancer can phone in to ask for information and share their anxieties, has been buzzing. Our counsellors are trying their best to allay fears but what can you say to those who feel their only lifeline has been abruptly taken away? The likelihood of an increase in mental illness is a reality, especially in a situation where people are cut off from traditional sources of support like the extended family, friends and colleagues.
Patients on palliative treatments are also having a hard time accessing the medicines and interventions they need to make their lives more bearable. One of our patients who went back to his village and could not get back has been in terrible pain since he ran out of his medication. When the family called our doctor, she could hear him sobbing in the background. It is to her credit that she contacted the local authorities who arranged for his medicines to reach him.
This is what all members of our palliative care team at CanSupport are doing today. Visiting patients who are very sick at their homes and delivering medicines and even rations to those who have run out and urgently need them.
As a palliative care service we are also very concerned about the plight of patients with COVID-19 who are dying alone in ICUs, separated from their loved ones. Not only does this deprive everyone of the need to say their final goodbyes but it is likely to lead to complicated grief. The rituals associated with death are essential for the grieving process. They fulfil a physical, emotional and spiritual need. The feeling that you are not alone requires the physical presence of others as well as the comfort of a kiss or a hug. That you can no longer do this in the present circumstances is likely to have lifelong repercussions.
It is also disheartening to hear that cancer screenings and new clinical trials are being postponed indefinitely. We know how even a few months delay in detecting a malignant tumour can reflect adversely on a prognosis of long-term survival. By stopping new clinical trials for which people have registered is like snatching away their last hope for a cure or remission. How ethical is this?
In 1994, I was awarded a Times of India Fellowship to study the role of alternative therapies in cancer. I had chosen this topic because, as a support person, I had been privy to stories of miraculous cures. I wanted to know if there was any factual basis to these accounts and whether these therapies (Ayurveda, homoeopathy, siddha, unani, yoga and naturopathy, among others) could be proposed as a possible alternative treatment for cancer.
My quest took me all over India and though I met several interesting and charismatic personalities, I found no evidence of a cure that could be attributed to any one of these therapies alone. Besides the fact that the practitioners did not keep adequate records, or follow up with those under their care, most patients came after they had finished their allopathic treatments or when the cancer had recurred and spread. They now needed palliative support.
But there was another bigger issue. No matter what I said, oncologists had a ready answer to dismiss these claims. It sounded convincing, "We cannot accept evidence of efficacy and safety unless proper clinical trials are conducted." This seemed a fair condition at the time though now, in the face of the Covid-19 pandemic, it seems to me that the same medical practitioners may have lowered their standards.
To sum up, I understand the need for extra precautions when treating people with cancer who are immune-compromised, but placing them in a situation where they have to choose between cancer and Covid-19 is unacceptable.