The Calm Before the Zika Storm

In 2007, in the small and remote island of Yap in the Federated States of Micronesia, people began to complain about rashes, conjunctivitis, and pain in the joints. Initial tests revealed that some had developed antibodies to the dengue virus, yet the signs and symptoms pointed towards something different.
In all, as the New England Journal of Medicine reported, there were 49 confirmed cases of infection in Yap, another 59 unconfirmed cases, no hospitalisations and no deaths.
Then it began to spread. Ignored by much of the global healthcare community, it moved rapidly to the Easter Island, Cook Islands, New Caledonia and Polynesia, breaking down healthcare systems wherever it went, but remaining limited in its virulence to the picturesque but remote Pacific Islands.
It was only later that scientists realised they were dealing with something almost unheard of—a Zika virus outbreak.
Prior to 2007, since its discovery in rhesus macaque monkeys in the Zika Forest in Uganda in 1947, only 14 documented cases of Zika virus infections in humans had ever occurred. And it had always been considered rare and relatively harmless to humans.
In May 2015, the Brazilian government reported its first case. A total of 16 people had tested positive for Zika. According to one theory, an infected traveller or athlete probably came to Brazil for the 2014 Football World Cup. A mosquito bit the traveller, contracted the virus, and went on to bite other humans, spreading the infection.
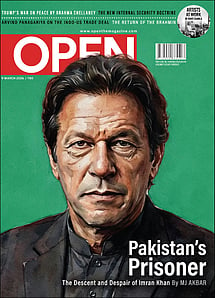
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
Since then, unfolding like a somewhat dystopian medical thriller, in a span of less than a year, the virus, carried and transmitted primarily by the Aedes aegypti mosquito, has run down the defences of more than 20 countries. It has infected an estimated three to four million individuals in the Americas, with around one million in Brazil alone.
Zika didn't just spread. It began to do incredibly weird and so far little understood things. The virus was known to transmit itself only through mosquito bites. Now doctors began to notice that in all probability mothers were passing on the virus to their foetuses, which strangely led to a condition known as microcephaly, where children are born with unusually small heads and incompletely formed brains. Some countries have even asked women to defer pregnancies till the outbreak is over. More recently instances of sexual transmission have been found. Some research has also found the virus in human saliva and urine, indicating that the virus can spread through them.
With the help of globalisation and the widespread distribution of the particularly hardy Aedes aegypti, Zika is now spreading into North America and Europe. The WHO has already categorised the outbreak as a public health emergency of international concern.
"There is no cure or vaccine for it. People don't even know what it exactly does," says Dr Kaushal Kumar, the former Joint Director and Head of the Centre for Medical Entomology & Vector Management, National Centre For Disease Control, who has spent several years studying various mosquito species in India. "And I think to myself, what if it reaches India. And by god, what hell it will bring."
Apart from increasing screening efforts at major airports, the Indian government has issued guidelines asking its nationals, especially pregnant women, to refrain from travelling to affected areas. The Pune-based National Institute of Virology (NIV) is currently screening samples. And the country's top medical research body, the Indian Council of Medical Research, has been asked to set up laboratories in case an outbreak occurs and samples need to be tested.
The NIV is currently screening dengue samples to check if the Zika virus might not have already reached Indian shores and be present in one of these samples. So far, according to Dr T Mourya, the director of NIV, all samples have tested negative.
Pointing out that mosquitoes are the largest killers in comparison to any other calamity or ailment globally, Dr Krishna Ella—a scientist and the founder of Bharat Biotech that is trying to build a vaccine for the virus—claims the potential for a Zika virus epidemic in India is incredibly high. He lists out how the Indian population is largely naïve about mosquito-borne ailments, and how the Aedes moquitoes that transmit the Zika virus are widespread in India and have already for several decades led to dengue and chikungunya outbreaks, as reasons for believing so.
Strangely, just after Zika was first discovered in monkeys in 1947 and before it was isolated in a human being for the first time in 1954, many Indians were found to be infected by the virus. A study, published in the Journal of Immunology in 1953, found that a total of 33 among 196 people had developed some form of antibody to the Zika virus. According to the authors of the study, later reported by the BBC, 'It therefore seems certain that Zika virus attacks human beings in India.'
What could this mean? Was Zika widespread among Indians long before this current outbreak? Does this mean India and the rest of the Asian continent represents a giant vulnerable population susceptible to Zika outbreaks? Or does it mean that Zika has been around and somewhat undetected in India for so long that we have developed some form of immunity to it?
According to Dr Om Shrivastav, one of Mumbai's top infectious disease specialists, it is unlikely, given these extremely early dates, that Zika was widespread in India in the early 1950s. "There is a lot being tossed about right now about the virus, much of it unscientific or unconfirmed. Even if it was Zika back then, we need to establish genomically that it is identical to the current outbreak," he says.
Dr Shrivastav's guess is that it is a case of cross reactivity, where the Zika virus is so closely related to other viruses causing infections like dengue and yellow fever, that the classic test—checking a patient's blood for antibodies that bind to the Zika virus—shows a false positive when it sees antibodies for infections similar to the Zika virus.
"For now there is no need to panic or be particularly worried really," says Dr Shrivastav, adding that he has been inundated with calls and queries about the Zika infection. "Just be careful and really watchful."
What makes India particularly susceptible to the Zika virus is its primary transmitter—the Aedes ageypti. Originally an African mosquito, the Aedes ageypti is believed to have spread across the world during the slave trade and the movement of ships and goods during the two world wars. In India, in its densely populated cities and tropical climate, this deadly mosquito species has muscled in and thrived, plaguing the country almost annually with huge dengue and chikungunya outbreaks.
"People say communalism, corruption and all these things are dangerous to the country," says Kumar of National Centre for Disease Control. "But I say, you've got it wrong. The most dangerous thing is this aegypti."
Among the 3,500 estimated species of mosquitoes that exist in the world, most of them feed only on fruits. It is only a few, including theAedes aegypti, whose females need to bite human beings to nourish their eggs.
In India, as researchers point out, urbanisation has been very good to the Aedes aegypti. This jet-black mosquito with white spots on its body can breed almost anywhere, from flower vases and plastic bags to tiny cups and tires with some water in it, from half-consumed coconut shells with a little rain water, as researcher Laxmikant Shinde points out, to an overturned bottle cap with a teaspoon of water in it.
They are also incredibly efficient in their business. Unlike most other mosquitoes, the Aedes aegypti are active even during the day. They usually hover low, bite an individual, usually on the legs and several times during each feeding. With each bite, the chances of contracting an infection increase.
They are also really difficult to exterminate. Shinde, the head of the zoology department of Jalna's JES College, says unlike other mosquitoes, the Aedes aegypti usually deposits its eggs in multiple well-hidden urban locations, thereby raising the odds of their survival. Many insecticides once used against Aedes aegypti are now almost worthless. "In the 1960s, we used to spray lots of DDT (dichlorodiphenyltrichloroethane). But now the Aedes mosquitoes have developed resistance against it," he says. "I have noticed that many of the insect sprays and repellents people use in their homes are also almost useless against the aegypti."
In India there has been little research to study the Aedes aegypti mosquito. "If you look at just Delhi," Kumar explains, "in the 1960s, all studies showed that the Aedes aegypti was restricted to the central and urban parts of Delhi, and the Aedes albopictus, the Asian mosquito, originally found in forests, and Aedes vittatus, were restricted to peripheral, semirural areas. This was the same when a similar study was conducted in the late 1990s. Now what you see is that while aegypti is still the dominant and most dangerous mosquito species, thealbopictus and the vittatus have also evolved and now breed within urban areas. In some cases, the two have been found to breed in the same pool of water.
The Aedes aegypti isn't also just a tropical mosquito in need of large modern cities like Delhi and Mumbai to breed in. They thrive almost everywhere including places like Dehradun in the north to small towns like Jalna in the west. Kumar has discovered several Aedes aegypti breeding grounds in seaports in Mumbai and Goa, and at both seaports and airports in places like Chennai, Bengaluru, Kolkata, Calicut, Cochin, among others. "This is really dangerous, because not only does the rest of the city become susceptible towards dengue and chikungunya outbreaks, but so does the rest of the world," he says. "Sometimes, like in the Mumbai port, the highest number of breeding grounds turns out to be things like buckets where they store water to douse out fires. One can just be a little careful and either keep the buckets shut or change water."
Between 2009 and 2013, when the small town of Jalna in western Maharashtr, began to suffer from an acute shortage of water like several other parts of the state, many residents also started suffering from dengue. "There are very few studies conducted here (in Jalna)," Shinde says. "But I was sure there was something interconnected between the two, water shortage and dengue." The head of the local college's zoology department then started examining public and residential areas within the town. "It was happening because people were storing drinking water. The Aedes aegypti, unknown to the people, were breeding in so many of them, from small earthen pots to large concrete tanks."
Dr Mourya of the NIV argues that the wide prevalence of the Aedes aegypti in India is no reason to claim that the Zika virus too will sooner or later reach Indian shores, pointing out that yellow fever, also carried and transmitted by the Aedes aegypti, never reached the country. But Dr Shrivastav thinks it is a faulty comparison, since there is a vaccine for yellow fever and we have successfully used it.
The wide prevalence of dengue and chikungunya in India, however, could have had one good trade off. An Indian firm has become the first company to file for a patent for two Zika virus vaccines. Last year, the Hyderabad-based company, Bharat Biotech, while trying to develop vaccines for chikungunya and dengue began working on a pair of vaccine candidates to protect humans against the Zika.
"Our interest in the Zika virus, an obscure virus when we started the project, was that the clinical features at an early stage of infection are indistinguishable from that of chikungunya and dengue… and (all of them) share the same Aedes mosquito vectors for transmission," says the firm's founder, Ella.
Pointing out that development of the vaccine is a long-drawn process involving five stages, including pre-clinical and clinical development, apart from seeking all government clearances, before endorsement for human use, Ella says, "We are concurrently working on two approaches… and one of them has reached the stage of pre-clinical testing in animals. Efforts are on in scale-up and characterisation of the vaccine product."
Even from an optimistic estimate, a vaccine could take a year or more. For now, options are pretty low-tech. "Be aware, use insect repellents, and always get rid of anything that could create a pool of standing water," Dr Shrivastav says. "And communities need to come together to become aware and remove mosquito breeding spots."