Interpretations of a Malady

New studies are telling us a lot about the distribution of cancer in India but not much about the reasons for it
In 2011, Indians suddenly heard that there was a new malignancy on the loose called sari cancer. Some media reports went along the lines of 'Beware women, wearing sari may cause cancer', others said it was a threat to women over 40. The search of that strange cancer led me at the time to JJ Hospital in Mumbai, whose doctor, according to the newspapers, was the one who discovered it. The surgeon turned out to be highly mystified and slightly disturbed. So far, he told me, all he had come across were three cases, and that too, spread over seven or eight years. He had not coined the term 'sari cancer' and did not like the panic that could be created. He had published a paper in a journal about two cases where rural women had waist dermatosis—roughening and eruption of the skin—that turned malignant. Often rural women screw the sari over one side of the waist tightly to make a bundle of sorts where they store things like money. The skin there turns rough, and in the three cases, he noticed that it had become cancerous.
"I reported it as waist cancer which occurred on the flank," said the JJ doctor. "Chronic irritation of any sort can lead to cancer." He had never seen it in urban women because they don't tolerate pain. The chance of contracting this cancer was almost zero for most women.
There was nothing called sari cancer, but like a self-fulfilling prophecy, the term came into common usage.
All ailments spread fear, but cancer is at a different league in making the human imagination cower. In How We Die, a bestselling book on death, the author Sherwin Nuland titles the chapter on the disease 'The Malevolence of Cancer' because there is nothing redeeming about it. He describes how the cells that turn cancerous behave like immortal juvenile delinquents feeding off the body without doing anything that contribute to the system like normal cells. The only purpose of cancer cells is to destroy life, 'raging against the society from which it sprang'.
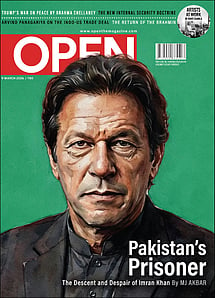
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
Complicating it is the fact that cancer is not caused by any one factor; a virus can lead to it, so can compounds in plastic bottles that your baby is feeding from and so can a piece of cloth continually rubbing against a part of the body for years. The indigent and the rich both get it but because of different reasons like poor hygiene versus eating too much. Children can get it but it is mainly a disease of the elderly. We live with the knowledge that cancer is always in wait, readier to pounce with every passing year. We take it for granted that cancer is increasing at an alarming rate in India. That might not necessarily be true.
At one of India's leading cancer institutes, Tata Memorial Hospital in Mumbai, Dr Rajesh Dikshit heads the epidemiology department and his job is to crunch the numbers that cancer research throws up. Dikshit headed the working group on cancer in the Million Death Study that was initiated by the Canadian-based Center for Global Health Research to study causes of death in India. The Registrar General of India monitors births and deaths in 1.1 million homes and for the study the surveyors were asked to ask for signs and symptoms of those who died. In 2012, a paper, 'Cancer mortality in India: a nationally representative survey', co-authored by Dikshit, was published and gave an all India picture of the disease. For example, a 30-year-old Indian man had a 4.7 per cent chance of dying of cancer before the age of 70, and for a 30-year-old woman it was 4.4 per cent. The most common fatal cancers in men were oral, stomach and lung, and in women it was cervical, stomach and breast. "The main cause of cancer deaths is tobacco," says Dikshit. It accounts for 40 per cent of all cancers.
There are things like this to be worried about but there is also another curious element—the number of cancer patients in India is increasing but the rate itself at which people are getting the disease is not really changing. Dikshit was part of another paper 'Cancer Incidence Trends in India', published in the Japanese Journal of Clinical Oncology this year. They looked at cancer incidence from six population based registries going all the way back to 1988 and also reviewed studies published over the period. The incidence rate is calculated by dividing new cancer numbers with the population. Because there is a difference in age patterns between countries (India is overwhelmingly young as against ageing Western nations) and cancer affects the elderly more, researchers also take into account age adjusted rates. Once that is done, it turns out cancer is not rising in any substantial manner in India.
The paper noted, 'No significant increases were observed by registries for all sites combined in either sex… even though there is a rise in the cancer burden—the number of new cancer cases in both sexes over the last two decades— corresponding incidence rates for all cancer sites combined may not have increased significantly.'
Dikshit's boss, Dr RA Badwe, director of Tata Memorial Hospital, who is a co-author of the paper, says that all cancers put together still follow more or less a straight line. In rural India, for instance, cancer affects 40 to 50 people per 100,000 per year. In urban India, it is around 100 per 100,000 per year. There is a rural-to-urban shift in the overall population, so the absolute numbers will increase. But the urban cancer rate has not risen from 100 per 100,000. The disease in its totality is almost constant, only society is changing.
Then there is the fact that cancer- wise India is better off when compared to other countries. A paper, 'The growing burden of cancer in India: epidemiology and social context', published in The Lancet Oncology this April, noted, 'GLOBOCAN estimates that about 14 million new cancer cases were diagnosed worldwide in 2012 and slightly more than 8 million cancer deaths occurred. 1 million of these new cases and nearly 700 000 of the deaths occurred in India, which is home to about 17% of the global population. Even in age-adjusted terms the recorded incidence for India is, at 94 per 100,000 people, only slightly more than half of the world average of 182 per 100,000, and about a third of that recorded in the more developed countries (268 per 100,000).'
So we are at half of what the world is suffering; even if the numbers double, we will only catch up with the mean. There is however a flip side to this— though Indians have less of a chance to get cancer, once contracted, they are in serious trouble. Says the paper, 'The cancer mortality rate in India is high, at 68% of the annual incidence.' For every 10 people who get diagnosed, seven die in India. Dr Mohandas Mallath of the Department of Digestive Diseases, Tata Medical Centre, Kolkata, and the first author of the paper, says, "The reason is simple. One million cancer patients a year [and] facilities to treat only 300,000. In my estimate only about 10 per cent of Indians have the finances to take adequate modern treatment."
The man responsible for a recent Times of India headline 'Cancer behind 70% deaths in India's atomic energy hubs' is the RTI activist Chetan Kothari. The first paragraph of the news report, based on his RTI application, says that cancer caused almost '70% of the 3,887 health-related deaths in the atomic energy hubs across the country over the last 20 years… In all, 2,600 succumbed to cancer in 19 centres between 1995 and 2014.'
Kothari had set out to search for suicide numbers and got cancer along with it. Curious about why a number of Department of Atomic Energy (DAE) scientists were killing themselves, he had asked the DAE how many employees died on duty, what was the cause of death and how many were suicides. Different DAE centres gave him the information separately. When I spoke to him, he seemed reluctant to take ownership of the 70 per cent figure. "I compiled [the replies to the RTI application from different centres] and gave it to the reporter. How they calculated, I don't know. It is 300, 400 pages," he says.
Kothari's ambivalence was partly because The Times of India had done a follow-up story two days later in which the Tata Memorial Hospital, which is under the Department of Atomic Energy, said that they had actually gone over the data and found the figure was 16 per cent and not 70 per cent. And even that could be on the higher side.
Dr Badwe has a simple explanation for the flawed interpretation of the data—this is a fallacy that comes out of extrapolating hospital numbers to the general population. The RTI application only got numbers for admissions that happened in DAE hospitals, he says. Cancer, being a chronic disease, will witness patients being hospitalised at some point whereas other ailments might not. If someone dies of a heart attack at home, his death wouldn't reflect in the data. "Those numbers are gone, so the denominator is chopped off completely," he says. "That doesn't mean cancer is more. For diabetes, nobody gets admitted, it is OPD treated. That is where selection bias comes in. Hospital based registries will give you a fallaciously high data."
Cancer is recorded in India in two ways—hospital based registries and population based registries. The former is important for administrators. "They are required for a person who manages the hospital. If I have a lot more patients of oral cancer then I should have a lot more facilities for treatment of oral cancer. Oral cancer may not be the most common cancer in the population, but I need to know what is coming to my hospital. If a lot more oral cancer patients are coming and I put a lot more money in colon cancer, that money is wasted," says Badwe. A truer overall picture of cancer may be got from population based registries. But there are issues here too. The Indian Council of Medical Research has 23 population based cancer registries in India, but an overwhelming majority are in urban areas. Dr Vinod Raina, director of medical oncology and hematology, Fortis Memorial Research Institute, led the Delhi Cancer Registry for five years. He says, "Population based data are more reliable. These are collected from household to household. Most of the registries, 80 per cent, are urban."
All the registries combined don't even cover 10 per cent of India's population. Fortunately, while they throw up regional anomalies that puzzle researchers, they also lead to agreement on many things. Dr Mallath says, "Some cancers are more common in some parts of India and some are rare. For example biliary and gall bladder cancer are very common in the north and eastern India compared to the west and south. Stomach cancer is more common in south and north eastern India. Cervix cancer is very common in all parts low in good water supply and [with scarce] private toilets. However, tobacco related cancers are common everywhere. We don't need more data to implicate tobacco as the cause of 40 per cent of cancer related deaths."
The most important trend in Indian cancer is breast cancer overtaking cervical cancer among women. It's like a seesaw: as breast goes up, cervical comes down. The latter is mainly contracted through a virus and so something as simple as personal hygiene leads to its decrease. Among Muslim women, for example, cervical cancer is at a very low level because most men of that faith are circumcised and circumcision protects them from the HPV virus whose transfer to women can lead to cancer.
Dr Sonal Puri, of the Department of Community Medicine at the Government Medical College and Hospital, Chandigarh, did a study of all the patients that came to the hospital over six months and found that breast cancer accounted for 23 per cent of all cases, followed by cervical. "Earlier, cervical was number one," she says. She is now doing a three-year study which has surveyed 4,547 patients and it too reflects the same thing.
One of the reasons for this rise in breast cancer is urbanisation and lifestyle changes. Says Raina, "Indians used to have large families and early marriage and early multiple pregnancies. That was protecting women against breast cancer. Now that our lifestyle has become Westernised, people have fewer children and they get married late and have children late, breast cancer incidence is increasing."
Urbanisation leads to a direct increase in some other cancers also. Badwe says, "One is breast cancer, second is ovarian cancer. Both these cancers rise remarkably. Lung cancer is on the rise in urban areas. So is large intestine cancer. These are all diet related or smoking related cancers."
A striking thing about cancer numbers in India is that we know a lot about their distribution, but very little about the why of it. For example, stomach cancer is more prevalent in the south, and while all sorts of explanations including the eating of pickles is hypothesised, no one is really sure why. Likewise for the high incidence of gall bladder cancer in the Gangetic belt. But Indian research in cancer is moving into etiology or causation only now, and slowly. Till the results come and more studies are done, cancer will continue to puzzle us.