The War on Microbes

It is time to call a truce—and get to know the microscopic animals inside the zoo that's the human body
Yesterday, like that celebrated feline, Erwin Schrödinger's Cat, I found myself in two states at once. I was at the Haffkine Institute, standing in the exact spot where man had declared war against microbes a century ago.
It was July 1897, and this corridor was a makeshift plague hospital. Six months earlier, Waldemar Haffkine had prepared his 'prophylactic against plague'. Nearly 8,000 people had been vaccinated, and very few had developed the disease. Here, walking up this very corridor, was Pasteur's celebrated pupil, Alexandre Yersin, the man officially credited with the discovery of the plague bacillus, armed with a 'curative serum' meant to treat the disease. Four patients received the injection that morning. It inaugurated an era. Just round the corner were magic molecules that would bombard microbes out of existence.
Today, a thriving mosquito farm occupies that plague ward. I walked past a nursery of rambunctious Culex larvae. A wire cage entrapped an angry anopheline whine: these malarials were hungry, straining for release. Rice plate was ready: a guinea pig blinked hopelessly in a box just slightly bigger than itself. With only a few turds for company, it existed for the sole purpose of being bitten once a week.
The young entomologist buzzing about cautioned me cheerily as he tapped the Anopheles cage. "Ever had malaria?" he asked. "Yes? Better watch out for bites, then!"
I thought I hadn't heard right. But he repeated the witticism with exiguous impatience.
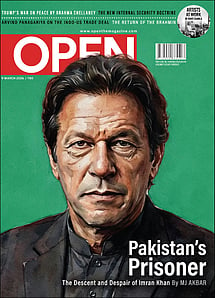
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
The truth sank in.
If I had Plasmodium in my blood, mosquitoes would find me irresistible.
And all along I had thought the shoe was on the other foot.
"That's just half the story," he corrected me.
Certainly, Plasmodium had infected my blood stream through a mosquito bite, but what was next? It needed to widen its horizons. Finding a new host could be an intelligent career move. Also, a neat scheme for going about that would be to make my sweat madly attractive to the Anopheles.
For the first time in half a century, I felt uncomfortable in my skin. I realised I might be oozing the mosquito equivalent of Chanel No 5. All on the orders of— what?— the malarial parasite? A tiny vacuolated blob of protoplasm lunching on my blood cells and burping away my haemoglobin? I hadn't expected my body to take orders from a microbe.
"Happens all the time," my new friend assured me with a grin. "Better get used to it."
Behind us, on the landing, busts of Louis Pasteur and Robert Koch were still standing, unperturbed. The oil painting of Haffkine vaccinating a crowd had not yet dissolved into teary smears. If Yersin had looked up, he might have exchanged a sly wink with them. Their moment had lasted more than a century.
One hundred years of sheer luck was the way I saw it now. For fifty of those, I had been indulged and sheltered and nourished by it. We were alive, I was alive, because of our war against microbes.
Now here I was, being pushed around by a scintilla of protein practically devoid of mass. All my weighty inheritance of science counted for nothing. It was a nullity, an illusion, no more. And yet, the moment I was confronted with a sick patient, it was my only reality.
The superposition of two completely different truths was difficult to grasp. The body was trapped in this entanglement, a biological verschränkung. How was I to come to terms with it?
Throughout the last century, science was drunk on conquest. We had drugs for every ill. We zapped the most horrific bugs with bigger, better, antibiotics.
When I was a surgical resident in the early 1980s, typhoid perforations, staph empyemas, and deep abscesses were all common emergencies. Burns always meant sepsis. Pus was everywhere; we mucked about in it, elbow deep. But we still wore a superior sneer, because, by then, tuberculosis was tamed. We used to pop into the TB Ward sometimes: it was a museum of failed therapies from an older time. Our parents narrated hapless tales of friends and relatives who had died coughing up blood in sanatoria. Panchgani, where I grew up, was dotted with these melancholy bungalows: they still wore a mephitic pall twenty years into the Age of Streptomycin.
Five years later, things got even better. Common surgical infections became uncommon. Complications, even rarer.
But by then AIDS had us worried—and we haven't stopped worrying since then.
We've woken up to new emerging diseases, pandemics some of them—and more than 70 per cent of these are zoönoses, diseases that properly belong to a different host species, and are now infecting humans.
Not that any of the old diseases have gone away. They're all baring their teeth anew. And fallen by the wayside are our trusty antibiotics, a new one is jettisoned every day.
We stand at the end of the antibiotic era. There are new monsters ahead, and the older monsters we fought now turn out to be friends. The newest science urges us to rethink the body.
What is sickness? What is health?
What does the body look like in this new understanding?
Is it individual or is it legion? And if so, who is for us and who against us?
Antibiotic resistance is the worst of nightmares, and every doctor faces it today. Of course, we're beating ourselves up over this, blaming our shot- in-the-dark therapies, our ill-informed choice of molecule, our lack of science in diagnosis.
Last August, an eclectic mix of the country's medical associations met in Chennai to form a strategy to review and respond to the crisis of anti-microbial resistance. The 'Chennai Declaration' calls for a complete overhaul in antibiotic usage. The road map for the projected seven- year timeframe has several intelligent signposts. Most crucially, it has not overlooked a critique of the medical curriculum. It reads well, and every doctor must hope it pays off.
But hope has no place in science.
What if, instead of looking for more complex weaponry, we chose, instead, to end the war?
The idea of a malarial parasite tweaking my sweat glands to hitch a ride out of my body was just a theory. It could be matched with a trillion other requirements of the gazillion other microbes— bacteria, viruses, protozoa, prions, even nematoda and insecta—that inhabit me. I haven't yet faced up to the fact, but that's what I am. That's what every human body is. It is an ambulant zoo. Talk of selfhood! Where, in this Rushdie-an ragbag of selves, is me? Let's face it, even my DNA isn't mine—my mitochondria are souvenirs of ancient liaisons with bacteria.
How ancient? About, say, 1.45 billion years old. However back in time we eukaryotes go, the microbe has an edge on us. A substantial edge, considering bacteria are almost as old as the planet. The recent sequencing of mitochondrial DNA from a 400,000-year-old skeleton from Sima des los Huesos in Spain may tell us much more than just where this ancestor fits in our family tree. Read differently, it might reveal the kind of world he lived in. Perhaps that isn't possible just yet, but we're getting there.
The body is a vibrant and sentient information network that functions quite independent of that old autocrat, the brain. All this time, while we've been hooked on puzzles neurological, microbes have been laughing up their lipoprotein sleeves.
Think of it: at least 6 taxonomic families of bacteria have squatters' rights on the human skin. These are commensals, literally supping at the same table; convivial fellows we've invited into our every crease and chink and crevice ever since we left the womb. They like the quiet life, and we don't notice them until they pack up and leave. Then we erupt into messy skin diseases.
It is good for the soul to consider these bacteria a workforce toiling ceaselessly for our welfare, but the truth might be just the opposite. They're here because it suits them. We're providing board and lodging and ensuring orgiastic frenzies of reproduction. What do we get in return?
Health, evidently.
Our much vaunted exoskeleton won't perform at optimum without its resident population of microbes, the skin microbiome. Texture, odour, colour, elasticity, all the sensuous delights of the skin are nothing more than the right microbe in the right place. There are different microbes that colonise different areas of the skin, and apparently, there isn't much difference between people.
At least, that's what we think now.
For all we know, inter-personal relations might be no more than the silent chatter of microbiomes. From first love to vendetta, everything might, quite literally, be skin deep.
And that's just the gift-wrapping.
Our visceral truths are far more disturbing.
The human gut carries about 100 trillion microorganisms. Most of the time, they're nice to us. They help us digest and absorb food, they ward off nasty microbes and maintain the highway when traffic comes hurtling down, after every meal, with a complex array of chemical signals. So helpful are they that in recent times, the end-of-the-road treatment for severe colitis is a faecal transplant.
That's exactly what it sounds like. It generally appears with a fancier label— FMT, Fecal Microbiota Transplantation.
The entire gut microbiome of the patient is replaced with donor faeces whose bacteria will now colonise the patient's intestine. This is easier to understand when you realise that the patient got sick in the first place because his gut microbiome was depleted or altered.
And the commonest cause of this is— antibiotics.
Without question, antibiotics tinker, tweak, and often injure the microbes in our intestines. Sometimes that can be disastrous, leading to super-infections by super bugs. While the immediate, and obvious, consequence may be diarrhoea or even a dangerous colitis, the more startling effects are now becoming evident.
The gut microbiome does not merely regulate the food industry in the body. It seems to be a major stakeholder in the brain.
That's not as bizarre as it sounds. The moment of exit from the womb marks the beginning of the most frenetic year of life. No matter how adventurous the years that follow, nothing can quite match up to the achievements of that first year. During this time, two events occur in tandem: the gut acquires its microbiome, and the brain develops at a staggering pace. Why shouldn't the two events be connected? Evidently they are.
Colitis of several varieties is associated with a slew of psychological illnesses— anxiety, depression, behavioural problems generally lumped together as stress disorders. What if stress is a microbial state?
The gut-brain axis is being avidly explored now, mainly in terms of neurological events. What if we looked at it from the microbe's point of view?
What must alter in the gut microbiome before something alters in the brain?
In Parkinson's Disease, brain cells contain a blob of abnormal protein called the Lewy body. The same anomaly is seen in nerves of the intestine in an early stage of the disease. The Lewy body is believed to be caused by oxidative stress. Genetic factors and environmental toxins conspire to produce it. The intestine is a serpentine sponge with a complex wiring of nerves close to its absorbent surface. So, could Parkinson's Disease begin in the intestine?
Medicine has thrown up stranger truths in the past. Still, there might be no end to the surprises in the next few years.
Bacteria are socially wired. They exchange information all the time by a nifty 'horizontal transfer,' which means they can transfer genes without hooking up.
The microbiome is a social medium that we still have to understand, but it is frighteningly sensitive. The bug in your mouthful of paani puri is on a blind date, but by the time it reaches the small intestine, it knows exactly where to set up shop. It has learnt all about you on the way. There's simply no privacy in the microbiome.
Commensals can bite, too. Much of their behaviour depends on the body's own response. In immuno-compromised people—who may have any illness from malnutrition to AIDS—the good guys turn traitor. They're still the commensal microbes they were, but now the body's response renders them pathogenic, and they produce serious, often debilitating, disease.
We've wasted a lot of time thinking we're the good guys and the microbes are badass savages that must be exterminated or controlled. That view is about as dated as the imperialist regimes that invented it, and we all know what happened to them. That tells the story, really, and it should end our war against microbes. We've been living too long with the enemy for apartheid. Time now to examine what makes our peaceful coexistence with microbes go wrong.
Imagine sitting down to dinner with a silent companion who ignores you. Wouldn't it make you mad? The Greeks probably invented deipnosophy, the gentle art of table talk, as much to avert enmity as to enhance the pleasures of the palate. Trillions of microbes sit at our table, waiting to be noticed. It is time now for conversation.
Actually, we have conversed before. But with the arrogance of new information, we've ignored or forgotten those exchanges. Recent discoveries should make us re-examine them.
For instance, the gut microbiome has three or four different varieties or enterotypes. Most people fall into these categories.
The bacterial profile of each enterotype is distinctive. This is exciting news for the evolutionary biologist. Should it also thrill the doctor? What does it mean in clinical terms? If the gut microbiome defines how many body systems work, what are the characteristics of people with different enterotypes? How do we recognise them?
Sound familiar?
It should. Especially in a country with a 3,000 year memory of defining prakriti as vata, pitta and kapha. All ancient and medieval systems of medicine recognise these humoral identities.
A medieval physician wouldn't dream of prescribing the same medication for ten people with the same disease. It would upset his very ethos. He was expected to prescribe as dictated by the 'type' his patient was; the natural state or prakriti was assessed not just by physical characteristics, but by personality traits as well. Shakespeare used this to remarkable effect in his plays where 'choler' and 'phlegm' have stellar roles.
Modern medicine dismissed these ideas airily the moment we discovered microbes. Perhaps that was exactly when we should have started looking more closely at them.
It is time to rethink the body.
It is time to rethink selfhood. And this time, with more latitude.
If our body is an ambulant zoo, we need to know its animals better. Or its animalcules, as Anton van Leeuwenhoek, the Father of Microbiology, preferred to call them.
Kalpish Ratna is the nom de plume of Bombay surgeons Ishrat Syed and Kalpana Swaminathan. Their book Once Upon A Hill is an itinerant history of Andheri's Gilbert Hill. Their novel The Quarantine Papers is now available in paperback