Booster Shot

In the late 19th and early 20th centuries, vaccines for pandemics like the Asian flu in 1957 and the swine flu of 2009 were developed well after the peak of the disease. But for Covid-19—one of the deadliest pandemics in history—several vaccines have been developed and approved within a year of the SARS-CoV-2 virus being identified. The vaccine developed at the Oxford University, one of the more promising ones, turned out to be 79 per cent effective against the disease and 100 per cent effective in stopping severe and fatal cases in trials conducted among 32,000 volunteers in the US, Chile and Peru, reported AstraZeneca, the university's corporate partner in developing the vaccine. However, some US federal health agencies have alleged that the Oxford-AstraZeneca team had revealed data selectively.
In their alacrity and level of global coordination, vaccine manufacturers have kept step with the pandemic. As medical experts have pointed out, research and development agencies of several countries, including the UK, Sweden and India, have contributed to fast-tracking approvals.
Shahid Jameel, virologist and director of the Trivedi School of Biosciences at Ashoka University, Sonipat, explains why the progress seems so rapid when compared with the past. "In earlier vaccines, the trials always happened sequentially. We first did research, and then it went into pre-clinical testing, and then clinical testing. Even the clinical Phases I, II and III went sequentially. Between every phase there were approval processes, which took time. It was only once the vaccines were finally approved did the manufacturing start."
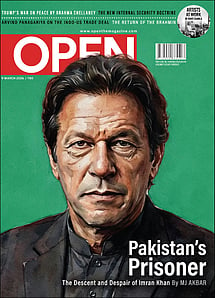
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
Jameel adds, "For the Covid vaccines, everything went parallelly. So, while animal studies were going on, regulators gave clearance for human trials. Phases I and II and Phases II and III were generally allowed together, and most importantly, the manufacturing facilities were built even before the vaccines were approved. For instance, the Serum Institute of India already had 40 million doses made and available even before it got approval."
Multiple factors contributed to this speeding-up, although the time taken for testing the vaccine on humans remains the same. As Jameel points out, "There was a sense of urgency even in 2003 when the SARS virus took place. It's just that the technology wasn't as advanced back then. Also, we did not have the platforms and funding mechanisms that we have today." He also stresses that even with the unprecedented speed, no shortcuts were taken for approvals.
Giridhar R Babu, epidemiologist at Public Health Foundation of India in Bengaluru, agrees, "There is a lot of regulatory process for the vaccines. This was observed all through the clinical trials. All these steps were taken and they had to be met with all the approvals and the guidelines of the ethics committee. The important thing was that no corners were cut, nothing was done to compromise the trials, even with the pressing situation of the pandemic."
In the past, vaccines were developed independently. Now, with so many companies and research institutions across the world coming together, they apply for various approvals together, leading to Covid vaccines coming out in just a year, about 10 times quicker than typical. Meanwhile, more vaccines are in the process of development, such as Serum Institute of India (SII)'s Covavax, in collaboration with American vaccine development firm Novavax, and CanSino, developed by Chinese firm CanSino Biologics in partnership with the country's military.
One crucial factor was that the facilities to manufacture these vaccines were already in place. Says Jameel, "No one expected so many vaccines to be made. Many countries and companies have the technology available to produce that kind of vaccine. The science is simple and platforms are available."
Though vaccine development has been rapid, the sequencing of doses is still being calibrated. Until recently, the prescribed gap between two doses of the Covishield vaccine, the Indian brandname for the Oxford-AstraZeneca vaccine manufactured by SII, was four to six weeks. However, on March 22nd, the Centre said that the period between the doses should be at most six to eight weeks. This follows studies published by the Lancet and World Health Organization (WHO) showing that the second dose is more effective with a longer gap.
Supporting the reasons behind this revised policy, Jameel says, "I think this directive has more to do with supply than with the science behind it. It's really driven by the availability of vaccine doses. In India at this time about 92 per cent of the vaccines given are Covishield and only about eight per cent are Covaxin. So Covaxin has not been made in amounts that we were expecting. A study published by AstraZeneca said that if you increase the period between the two doses to eight to 12 weeks you get better efficacy. But with the surge in India, it's important to get the vaccine into as many people as quickly as possible."
According to some experts, earlier studies released by AstraZeneca and others also recommended a gap between doses of six to 12 weeks. The Indian Government had initially advised a gap of 28 days, later increasing it up to at most six weeks.
Like Jameel, some experts support India's revised policy saying that more people can be vaccinated if the gap is longer. Babu says, "WHO has already recommended eight to 12 weeks, as has the Lancet study. The US announced 28 days. Any duration with the minimum of four weeks to 12 weeks is a safe margin. These intervals, the longer they are, will allow more people to get vaccinated."
Not all medical professionals, even when endorsing the Centre's decision, agree with this reasoning. One Delhi-based professional says on condition of anonymity, "Increasing the gap between doses should have been done a long time ago. The studies done by WHO show very clearly that the response of the antibodies as well as the efficacy increase eight weeks after the first dose. This is a continuum. The longer the interval, ideally up to 12 weeks, the better is the response. Before the regulation, many have pushed their doses to the second week. The decision has nothing to do with vaccine shortage. It is clearly a decision based on the scientific evidence."
The expert adds, "This evidence was available a month ago. When an individual is given the first dose, they develop antibodies, and it is possible if they are given the second dose too soon after, the response won't be as effective due to the antibody production of the first one. Biologically also, it is better to space out the doses of this particular vaccine."
There is now evidence, many experts claim, from the later clinical trials that the longer the interval, the better the effect, as reported by AstraZeneca. The expert says, "One reason the Government is not pushing it is that there are two vaccines in the market, and for the second vaccine, Covaxin, the evidence available is for a 28-day gap."
Doctors also fear that if secondary infections begin showing, people will become reluctant to take the second dose. The Delhi-based expert warns, "One dose is not protective. There are people who can get a Covid infection after one dose. There are two reasons for this. One is that the body has not developed the full immune response. Also, many people have stopped taking precautions (no mask or physical distancing); plus there is another surge. The pandemic won't go away until personal behaviour changes. There's a quantum jump as you cross the eighth week." The expert adds, "Each peak is worse than the last one. There are new variants of the virus in Punjab, like the UK variant."
The general public is still unsure about which vaccine is better. But Babu says, "All vaccines have shown reasonable safety and efficacy. All the vaccines are good, as they have proved they can prevent deaths."
As Jameel observes, "The vaccine that you get in your arm is the most effective vaccine. It's unfair to compare vaccines because vaccines have not yet been tested against each other. The efficacy of 90 per cent as compared with 70 per cent is really an artificial comparison. This is because the number is for that duration of time for which you have the data. So if you have the data at two months' time, that essentially tells you the efficacy for two months' timepoint. It doesn't mean the same efficacy will remain for, say, five years. Many people don't understand that, and they can only stick to comparing 70 per cent with 90 per cent. The important thing is to get a vaccine straight away. All of the vaccines which have got any kind approval have met the 50 per cent efficacy point that WHO set when vaccine development started."
Is there a possibility of a single Covid vaccine emerging?
Jameel does not think so: "That won't happen as there are already around 70 vaccines in various stages of testing. At least a dozen vaccines have been approved in several countries." He sums up the debate around this: "The good thing is with so many people, so many companies getting so many vaccines, it really bodes well for the future and any future epidemic or pandemic we might face. Why rely on one, when you have a bouquet of vaccines?"