Notes to Ourselves

What must we do to survive the persistent onslaught of dengue, malaria, chikungunya, swine flu…?
The city is a jungle—hotter, wetter, darker than it used to be. There are predators about.
This month, in a shanty in a Bombay suburb, there were two deaths. The first, horrific and brutal, left the city stunned in disbelief. The second was a private grief. It was no less horrific and brutal, but it passed unnoticed, except as a hospital statistic.
Both victims were girls. Both were two years old. Both bled to death. Both were killed by predators.
Their predators were very different. One was a leopard, the other a mosquito.
Both predators attacked for the same reason: the city is a jungle now—hotter, wetter, darker than ever before.
The leopard attack is easy to understand. Encroaching on a big cat's habitat can have only one possible fallout. And it is always the poor, deprived of sanitation, who pay the price. The parents of this child were reprimanded for letting their child out in the dark. Nobody blamed the state for the lack of sanitation.
The mosquito attack is less obvious. After all, we have always had mosquitoes, malaria and vague fevers that occasionally acquire exotic labels. Mosqui- toes are a nuisance, but nobody in their right mind would call them predators.
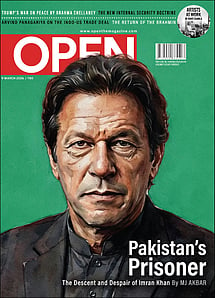
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
It would be more correct to call them vectors for organisms that cause frightening, sometimes fatal, diseases. Malaria, dengue, chikungunya, yellow fever—and, we're just getting started. The truth is: none of these organisms would infect us if we weren't bitten by mosquitoes.
That girl who was bitten by a mosquito bled to death from DHF (Dengue Haemorrhagic Fever), a death every bit as gruesome as being devoured by a leopard.
If statistics be trusted, 3 billion people on our planet are at risk of being infected by the flavivirus that causes dengue fever. Of these, 2 million will develop the potentially fatal haemorrhagic form, DHF. Of these, 20,000 will die deaths as terrifying as that little girl's. Also, most of these 20,000 who die will be children.
No, there is no vaccine as yet, and not for want of trying.
There are four infective serotypes to the virus that causes dengue. A serotype is a variation within a species of virus. All of them, or some of them, or one of them, can enter the bloodstream after a mosquito bite. There is no cross-immunity between serotypes. If you were infected by one serotype, the other three are still queued up inside the next mosquito getting ready to lunch on you. So any vaccine, to be effective, must provide immunity against all four serotypes. This is not easy to achieve. The first clinical trial is on, but it may be years before we have a vaccine that works.
Meanwhile, there is no treatment for dengue. All we can do is be vigilant against complications, and treat those when they occur. Past that, we do the best we can, on a wing and a prayer. Because these complications are operatic multi-organ disasters, where the body leaks plasma and bleeds into itself, doctors know that even if they win a few battles, they are still losing the war.
This year, almost every Indian metropolis manifests dengue. Nothing newsworthy there, we have had dengue since 1780, when an epidemic swept through Madras. We first isolated the virus in Kolkata in 1944 in the blood of US soldiers. DHF was first recorded in the Philippines in 1954-55. It took thirty years to get to India, and we have had sporadic cases since 1988.
The first epidemic of DHF occurred in 1996 in northern India, and since then, it has left no part of the Subcontinent untouched. A recent 50-year profile of dengue in India shows a drastic change in pattern. Earlier outbreaks were sporadic, and restricted to large cities, and there were few severe cases. Things are different now. Dengue has become endemic to the Subcontinent: this simply means it is everywhere, all the time, and, as bad as it ever gets.
We need to ask why.
About every hundred years, and usually at the height of an epidemic, exhausted by useless endeavour, medicine asks itself this question. Or needs to.
The last time it did so, we discovered microbes and germ theory, invented antibiotics, and congratulated ourselves. 'We have conquered disease!' we said.
For the next fifty years, we almost did. But in our complacence, it took us another fifty to notice otherwise. Not only were old enemies, like tuberculosis, back with renewed malignance, but there were other, entirely unexpected, new ones.
Where did they come from? Apparent-ly, from others who inhabit the earth.
More than 60 per cent of the organisms known to cause disease in humans reach us through other species. In the past few years we have learnt that the hard way through swine and avian flu, encephalitis and BSE (bovine spongiform encephalopathy aka mad cow disease). That is just what we saw up close.
The long view is more paranoiac. Every class, genera, phylum, species among animals appears to be poised against Homo sapiens, and in a rush to foist us with disease. The plant kingdom is holding back—but for how long? It is only a matter of time before the banana bites back.
Some of these diseases are zoonoses. They are caused by organisms that primarily infect other species, but are transmitted to us, directly or through a vector. Many do not necessarily infect other species, but once they enter the human body, through a vector like the mosquito, they leave us dangerously sick. The mosquito is a promiscuous biter, and can transmit infection from one host to the next.
Our reaction to this understanding has been—I was going to say brutish, but I'll amend that… our reaction has been intensely human. We have, thoughtlessly, reached for the gun. We kill, massacre, cull, and just as we think we are rid of crows, chicken, swine, rats, mosquitoes, we are bitten by an entirely new entity.
A little hindsight might help here.
Through the 19th century, epidemics and famines alternated each year and decimated millions of Indians. Most of these epidemics emerged after massive assaults on the environment. Of course, they were not called that then. It was all well-intentioned progress: mountains were stripped bare, hills flattened, rivers dammed. Tree cover was lost, and there was eutrophication (the increase of nitrogen and phosphorus containing matter in water due to an overload of organic waste) of water bodies. Drought, famine, epidemics followed. The cycle never varied.
We need to remember that now and match it against ground reality.
A recent study of a decade of dengue in Delhi revealed peak incidence in 2010—a year marked by massive construction to overhaul the city for the Commonwealth Games. Mumbai, striving for verticality, has been in constant upheaval since the turn of the century. It has become hotter, with more people squeezed into less space. It has become darker—the roads are now dim labyrinths in the shadows of humungous concretisation. It has become wetter, even though the monsoon failed this year—there are puddles of stinking stagnant water everywhere. These verities confront us each day.
What do they mean to the mosquito?
Aedes aegypti, the mosquito that transmits dengue, loves it here. Perhaps it started off in a distant jungle, but for the past century, it has been an urban sophisticate. It likes it hot. It thrives best between 21ºC and 29ºC. It gets eggsy as it warms up. It loves the damp. The eggs hatch when they come into contact with water. It cosies up to humans in shadowy interiors and gloomy roads. It is a day biter, and only the female is a blood feeder. She needs a long cool sip of plant nectar for a few days before she graduates to blood. She needs a high energy concentrate to lay an incredible 500 eggs over her short lifespan of two weeks, and human blood fits the bill perfectly.
How does she find a host?
She sniffs us out with two smart sensors: the first detects CO2, and the other, the human odour she finds irresistible. Apparently, it is the CO2 that makes her a happy hunter. It sensitises her to home in on the host even if that savoury odour is very faint. The brighter and greener the surroundings are, the lower is the CO2 level, and lesser the chance of being bitten by Aedes. Indoors, and with no plantlife to sponge up the CO2, Aedes will get you every time you exhale.
She lays her eggs, preferentially, in non-biodegradable plastics, jars, bottles and drums, all waiting to be filled with vivifying water. And those eggs can wait a long time, months sometimes, before they hatch into hungry larvae. A city dump in the midst of human habitation is an Aedes Garden of Eden.
Once she sinks her proboscis into human skin, Aedes bloats to twice her body weight with the blood she imbibes. A good meal can get her to lay a hundred eggs over the next few days. That is a lot of dengue to live with.
The official response to dengue is not intelligent. Every evening a noisy permethrin fog sets the city wheezing. It deters Aedes not a bit, but something is being done! The racket, the stench, the cough and their watering eyes assure taxpayers that their money is hard at work.
In hospitals there is a flurry over lab tests, diagnostic kits, prognostic scores. How many of these actually help?
In the first four days of fever, dengue is confirmed by either virus isolation or RT-PCR (Reverse Transcription Polymerase Chain Reaction). After day 4, the diagnosis is based on sero-conversion—immunoglobulin levels in the blood. A sample drawn in the third week of illness must be matched with one drawn on day 4 or 5. That makes it of little use in a patient who only sees the doctor after he has been ill for a week. Most hospitals in India have developed their own prognostic scores as symptoms vary, and WHO grades do not work.
Finally, it all comes down to the physician's clinical judgment. This, the doctor's most reliable tool, and often the only one, cannot be computed. Today's patient will not buy that.
'It's dengue because I say so,' may be misconstrued as arrogance, not skill. As with other illnesses, the defensive practice of medicine overburdens the laboratory.
Faced with a killer disease for which there are no tests and no treatments, what are we left with? Research? Sure. Wonderful work is being done by serologists, virologists, entomologists and botanists—in laboratories and in the field, and much of this should be of immediate practical significance. We are learning about plants that can be powerful pesticides. But we fail to question why we do not have them in use. We are discovering points of vulnerability in Aedes aegypti.
We know their larvae feed on rotifers in discarded plastic waste. Bdelloid rotifers, a celibate sisterhood, withstand almost every form of deprivation: heat, drying, ionising radiation. Get rid of them, and the Aedes larvae will starve to death. This does not seem practical.
But the elimination of those veritable mountains of plastic waste our cities produce is certainly something we can work to achieve.
To disable adult mosquitoes, surreal methods are being crafted in sophisticated laboratories: some render the males sterile, others mess up the female's digestion so that a blood meal will sicken her.
Reading these reports triggered off a childhood memory of dusk in Calcutta. Night fell abruptly and we had to hurry home from play. The air stung with smoke from the sigdis being lit to cook dinner. As we ran home, each of us would have an interested column of mosquitoes whizzing over our heads, they followed us all the way home without breaking formation. Sometimes we skipped and danced around in attempts to disperse them, but they would always, always, fall right back in line.
Mosquitoes are inevitable. We have lived with them since we arrived on the planet, and, they were very old money even then. They are smarter than us. In evolutionary terms, they adapt faster to change than we do.
Most of the species that carry or transmit disease have been cheated out of their sylvatic existence. Like rats, mosquitoes have become urbanised and domesticated. They are vagile, they are cosmopolites used to intercontinental travel. Any disease they harbour is a potential pandemic.
We will not be able to exterminate mosquitoes, just as we will not be exterminating cows, sheep, swine, chickens, crows, civet cats and chimpanzees any time soon. Is it not time for a détente?
To stop this tsunami of zoonoses that looms, we must learn to coexist with other species. Our civic decisions must respect their habitats—and our own.
Nothing democratises a city as quickly as disease. A recent study shows Aedes aegypti happily ensconced in high-rise buildings. That poetic justice serves to remind us that it is the high-rise that created the slum next door to its dump. Building projects so recklessly approved by the municipality are death warrants, most of them. Land laws must be revised to prioritise health hazards, and the blame for every epidemic placed squarely on civic mismanagement.
India alone registers between 50,000 and 100,000 cases of dengue a year. Yes, it is true, only a small fraction of these will progress into DHF. But even without that complication, dengue is not just another fever.
Several months ago, transiting through Haridwar gave me a modest bout of dengue. The fever has left me with a harsh headache behind the eyes that I still have not shaken off.
Mine was a mild bout, and when I visited, Haridwar was practically empty. The Kumbh is now at hand, and I do not like to think of how Aedes aegypti will revel in it.
Global warming has a curious effect on insects in the tropics. It increases their metabolic rate. This means they are hungrier, sexier, eggsier. And, there are more of them.
With more carbon emissions, more plastic, more vectors, the urban concrete high-rise is the new jungle—hotter, wetter, darker than ever before.