The Birth Pangs of the Indian Male Contraceptive

IT WAS SOMETIME in 1984, when RS Sharma had just joined the Indian Council of Medical Research (ICMR), that he first learnt about the proposal of a non-surgical male contraceptive. It was instantly appealing. Not just because this drug was so easy to administer (injected into two sides of the scrotum), and would, in theory, render infertility for several years, but that its effects could also be as easily reversed (another two shots). This was a period when the ICMR was seeking out proposals for a male contraceptive to tackle the issue of the country's burgeoning population. And Risug (an acronym for Reversible Inhibition of Sperm under Guidance), developed by Sujoy Kumar Guha, then a professor at IIT Delhi, was one of several promising ideas.
A little more than a month ago, more than 40 years since it was pitched, and about a year after his retirement from ICMR, Sharma finally published the Phase 3 clinical trials of this contraceptive. "There were just so many delays," Sharma says over the phone. "We had to start the trial afresh once, another time the drug became unavailable. But we were finally able to complete it."
The performance of a drug once it is put out into the real world of course varies from observations made during a clinical trial. But the results of this trial have been so stellar, Sharma says, that if and when Risug becomes available publicly, he thinks it will rank, in efficacy, among the very best contraceptives available.
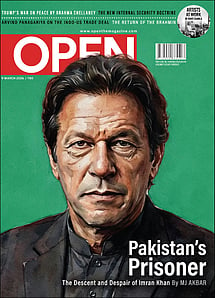
Imran Khan: Pakistan’s Prisoner
27 Feb 2026 - Vol 04 | Issue 60
The descent and despair of Imran Khan
"From what I have seen, I can say, this is going to be one of the most effective ones out there," he says.
The development of a male contraceptive drug has never been a priority. A vast number of options have been developed for women, from birth control pills and intrauterine devices to implants and vaginal rings. But for men, there are just two—vasectomies and condoms. Globally, vasectomies have never been a popular choice. In India, its use is particularly rare. They made up for just 0.3 per cent of the birth control methods adopted from 2019 to 2021, according to the fifth National Family Health Survey. By comparison, female sterilisations (or tubectomies) made up 37.9 per cent. Condoms are used but they aren't the most effective at birth control—the Centers for Disease Control and Prevention in the US estimates a use failure rate of 13 per cent.
Men should have equal responsibility to prevent unwanted pregnancies but the burden of birth control has always largely fallen upon women. In the last few decades, however, there have been attempts to develop a male equivalent of the birth control pill. Most of these, like the female counterpart in the market, were hormonal in nature, and while showing promise during trials, they were found to cause side effects such as irritability, mood swings, weight gain, and acne. This may sound par for the course, given that the female birth control pill is known to cause similar side effects. But this was reason enough for most organisations and companies searching for male birth control pill to either put it in cold storage or shelve it completely.
A few more are currently being looked at. These range from a contraceptive developed by researchers at the University of Minnesota in the US that targets a protein that plays a vital role in sperm production and fertility, to an injectable hydrogel that has been described by its developer (the American biotech firm Contraline) as an IUD for men, to a hormonal gel (funded by the National Institutes of Health in the US) that is applied on shoulders and upper arms once per day. But most of these are still undergoing trials, and even if found effective, are several years away from development. Of these, Risug, first proposed decades ago, is now the first one off the mark. Its latest and final Phase 3 trials, which followed 303 men injected with the drug for seven years, found that it is both exceptionally effective as a contraceptive and extremely safe.
Risug consists of a polymeric agent (Styrene Maleic Anhydride or SMA) in what is described as a vehicle of Dimethyl Sulphoxide (or DMSO). Administered on two sides of the scrotum through the form of an injection, the drug forms a small and flexible filter in the vas deferens—the duct that produces sperm—and disturbs the inherent negative surface charge on spermatozoa. The rupture this causes on the spermatozoa's acrosomal membrane, the subsequent leaching of the enzyme, and the acidifying property of the SMA results in making the individual infertile.
An earlier restricted Phase 3 trial, published in 2019, which followed a smaller and different cohort of 139 married men under the age of 41 for a period of six months after they were injected with Risug, also exhibited promising results. That study was also carried out by the same set of researchers. Then, out of the 139 participants, 133 had either low sperm count (oligozoospermia) or no sperm (azoospermia ) within a month of being injected with the drug, and this remained so even six months later, and none of their wives became pregnant after having unprotected sex. The drug failed to induce oligozoospermia or azoospermia in six participants, but this was caused, the researchers explained, because the required dose of the drug had not been injected.
The current paper, which Sharma describes as the final Phase 3 trials, was published in the journal Andrology. It follows a different and much larger cohort of 303 men across five states injected with Risug over the course of seven years. The researchers found that 92.7 per cent of the subjects achieved azoospermia within two-and-a-half months of being injected with the drug, which then increased to 97.2 per cent at the sixth-month mark, and thereafter to the highest level of 97.3 per cent at the one-year mark, and stayed that way for the entirety of the seven-year period. In 99.02 per cent of the cases, none of their wives became pregnant. Although the paper shows the results of individuals followed till the seventh year, in the other smaller group whose results he published in 2019, he says, he found the drug remained effective even in the 13th year. No serious side effect was also found. "These are very good results," Sharma says. "It is both safe and highly effective, and shows all the features necessary for a method to be in a mass family welfare programme."
A total of eight pregnancies were reported during this current study. Three of these were caused, the researchers say, because of the failure in the method of injecting the drug, and just one was caused by the drug's failure. In the remaining four, attributed to social causes, the azoospermic husbands weren't behind the pregnancies.
Animal trials have established that the effects of Risug can be reversed. However, this aspect has not been studied in human trials.
TO SHARMA, AS a researcher, one of the biggest challenges that confronted him was finding enough participants to enrol for the study. Initially, the researchers approached men who were turning up at family planning clinics and departments of urology or surgery in hospitals for vasectomies and no-scalpel vasectomies. "But very few men opt for vasectomies, and we would find about 10 men or so showing up at these centres monthly. Out of these, maybe one or two would agree to get injected with a new drug like Risug," Sharma says. "At this rate, I realised I won't be able to enrol even 300 subjects in 10 years."
So, the researchers changed their approach. Adopting what Sharma calls the "camp approach", the researchers would set up camps in villages and urban centres, and approach community leaders and individuals to convince more men to give this new drug a shot. "We reached out to around 700 or 800 subjects this way, I think," Sharma says. Out of these, 358 individuals fulfilled the study's inclusion and exclusion criteria, but a few had to be eliminated from the analysis of the study, because they either could not be traced during follow-ups or because they appeared to have violated some of the study's protocols.
The 303 subjects that were finally included in this study's analysis hail from five different states and belong to various religious and caste groups. This is important, Sharma says, to find out whether a drug is equally effective across different populations. Many of the participants were Muslims, and this shows, Sharma says, that the drug will find acceptability by members of that faith too, several of whom otherwise shun vasectomies believing it to go against religious doctrine.
Finding enough individuals to enrol for the study, however, was far from the only problem.
Sujoy Kumar Guha, the inventor of Risug who is now 83 years old, carries the reputation of a maverick scientist. I had first spoken with him many years ago about an unpublished study the ICMR had once conducted. There had been frequent reports then of condom slippage in India, and the ICMR had worried if this wasn't because there was a discrepancy between condoms, which are made to global size specifications, and the size of the average Indian penis. A study to measure Indian penises was then commissioned, but convincing men to unzip and offer their aroused members for measurement was easier said than done. Guha came up with the idea of a digital camera, which a man could use to take a picture of his erect penis in private, and a specially-developed algorithm that could process the data captured by the camera to arrive at the exact measurement of the penis in question. Guha's camera trials were a success, but the method proved too costly for the ICMR study.
His work with Risug however is way older. He first published a paper about such a contraceptive drug in 1979. There were however several obstacles, from individuals who raised concerns about certain carcinogenic components being used to traces of albumin being found in urine samples. These were unreasonable fears, and all of them were dismissed over time, but each caused more delay. "Tactics where a scare is created that some compound is carcinogenic in nature is a standard practice. It is used by [drug] companies to stop another company," Guha says. "Companies know how to tackle this issue. But we are academics and we did not know [how to deal with it]."
At one point when the trial was stuck in 2002, Guha managed to get an appointment with the then President APJ Abdul Kalam. It was 12 in the afternoon at the Rashtrapati Bhavan in September 2002, and Guha had been allotted 15 minutes with the president. "He listened patiently to all I had to say. Then, he said, 'Professor, you have run into a block. And this is not a scientist's block. I will tell the health people, but I do not expect much from them. You get a company and they know how to manoeuvre things.' And on the table, Kalam moved his hand like a snake does, and said a company will know how to go around this thing," Guha recalls.
By the evening, a meeting with the health minister was set up for the following day, but as Kalam had predicted, the ministry wiggled its way out of granting approval for the trial. More promisingly, later that same evening, an ADC (aide-de-camp) of the president showed up at Guha's quarter in IIT Delhi with a representative from a pharmaceutical company. The company agreed to come on board and things appeared to look better again, but after a few months, a lobby that did not want Risug to go ahead, Guha says, caused a problem by targeting another drug of the same company. That company probably read the leaves in the teacup and withdrew from the Risug collaboration.
Approvals eventually came through, but several years had gone by.
The biggest issue with Risug, it appears, is that it is too good for its own sake. Firstly, producing this drug, as Sharma points out, is a complex task. And, equally importantly, a drug that only needs to be injected once to grant years of lasting protection, is not one that will entice pharmaceutical companies with promises of high profit margins.
This was noticeable right from the outset of this drug's development. The Phase 3 trials of the drug had initially begun in 2000, and the first batch of individuals had even been injected. Still, the international protocol for the approval of new drugs was suddenly changed, leading to the trial being reinitiated with a new group in 2007. The pharmaceutical major Glenmark Laboratories had signed up to manufacture the drug and had even manufactured one batch, but once the company realised the complexity of manufacturing this drug and the low profit margins it would probably yield since it provided lasting protection, Sharma says, the company stopped producing the drug. "For the next four years, we could not get any company on board," he says. The drug had met a dead end once more. From 2008 onwards, right up to early 2012, the study could not be carried out, because no drug was available.
One of the problems this caused was that while Phase 1 and 2 trials can use drugs manufactured in a regular lab, for Phase 3 clinical trials involving humans, it is mandatory that the drug in question is manufactured by a company. A solution had to be found. But this time, the government took the lead. Guha was asked to set up and register a private company, which was really just a centre for the production of Risug, and ICMR got IIT Kharagpur to allot some space on its campus for it. "It was a brilliant idea by the ministry of health and ICMR. It was just a kind of paper company. And with that, we manufactured the drug for the trial," Guha says.
The study was completed sometime around 2019. However, the delay caused by the pandemic meant Sharma could only return to analysing the data last year. By then, he had retired from ICMR (where he served as the head and senior deputy director general in its Division of Reproductive Biology, Maternal and Child Health) and taken up the job of a distinguished professor at the Department of Biotechnology, School of Engineering and Technology in Greater Noida's Sharda University. Guha had also moved to Delhi by then, and he was even awarded the Padma Shri in 2020. The Risug Centre at IIT Kharagpur is still present, but it is not functional anymore. In 2019, the IND (Investigational New Drug) Committee, which is chaired by the director general of ICMR and the secretary of the Department of Health Research (Balram Bhargava), finally granted permission, Guha says, to manufacture and market the drug.
The obstacles to introducing a new method of contraception into the market however still remain enormous. Risug will need a pharmaceutical company to bring it to the market, and in the past, the industry's support for it and other male contraceptive proposals have been tepid.
Given these challenges, what are Risug's chances really for it to ever hit the market?
"I am not only hopeful but very confident it will be so [available in the market]," Guha says. His hope stems not just because of how effective it is, and that it is so easy to administer and can probably be reversed, but because he has realised that the drug and the technology behind it can have many more applications.
Guha, for instance, has been approached for adapting Risug to control the stray dog menace in the country. Before clinical trials on humans began, successful trials on rats, rabbits, and two species of monkeys were also carried out, and Guha sees no reason why it won't work on canines. The Municipal Corporation of Delhi was the first one to approach him for this end. After it was examined by a committee, it was passed in Delhi's Legislative Assembly, but the Covid pandemic broke out before it could be put into action. The Union Ministry of Fisheries, Animal Husbandry, and Dairying is now considering using Risug, Guha says, as a possible method to conduct mass sterilisation campaigns for dogs, and is soon about to start a study in Mathura's DUVASU, one of the largest veterinary universities in the country. A little while ago, Guha even found himself in the office of the industrialist Naveen Jindal, who had invited him and wanted to help in the application of Risug to deal with the stray dog population.
The current process of sterilising stray dogs is a long and expensive process. As Guha explains, dogs are captured from a particular locality and taken to an NGO with facilities to conduct sterilisation. Here, they are made to recover for a few days after the surgery is performed, before being returned to their original locality. "This whole process takes six to seven days. But I have worked out a different scheme, where you have a special surgical van. This van will be stationed in one locality. A dog once caught will be taken to the van, given a little anaesthesia, and within seven minutes or so Risug will be injected into the dog, and that dog will walk out from that vehicle. From a 6-to-7-day procedure as it is now, using Risug, we can cut it down to 7-to-10 minutes," Guha says. "This way, all the dogs of the city of Delhi can be sterilised in six months' time."
Guha has also developed a version of the drug that can be used for women. Here, Risug is administered using a probe through the vagina and into the fallopian tubes. He developed this method, which is minimally invasive, he says, because, during mass sterilisation camps (where tubectomies are performed), there are often reports of infections and sometimes deaths, as happened at one such camp in Chhattisgarh in 2014 when 13 women died and several more were hospitalised in a critical condition. He is now looking to develop a simpler probe, something for which he has applied to the ICMR for grants, before he can take it forward for human trials. "At present, what I have is a bit complicated. I'm looking to work out a more convenient probe, something which can be used by a doctor even in a primary health centre," he says.
He is also investigating several other promising applications. These include exploring the promise it has shown as a way to stop an HIV-infected man, when he is injected with the drug, from transmitting the virus to his sexual partner; and even using a modified version of the drug, which he calls RISUG adv, which when injected into the vas deferens, forms a nano-drug that goes to the prostrate and shows the potential of preventing mutation that causes prostate cancer. For the latter, while he has applied for funds to take this proposal forward in India, he has also teamed up with a scientist abroad who has got permissions to conduct a small clinical trial in some countries in Europe.
Guha may be 83, but he is in no mood to slow down.
Contraception remains an unshared burden. The market, and even governments' family planning projects, usually target women. They, after all, face most of the consequences of unplanned pregnancies. For a pharmaceutical company, a male contraceptive will only make financial sense if they are certain that men will embrace it. Will men be willing to do that?
"It is a new type of contraceptive. I think everyone from social organisations and NGOs involved in family planning to the government will have to help take this product forward and explain it to people, and make men understand that they too need to share the responsibility [of birth control]. If you do it, I think it will do very well," Sharma says. "This is a world-class product."